Aligning Healthcare Startups with Current Industry Trends
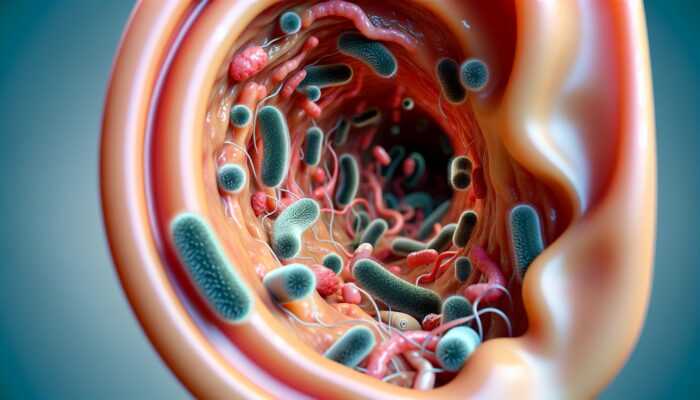
Comprehensive Insights into the UK Healthcare System
The UK healthcare system is a multifaceted and intricate landscape that offers substantial opportunities for healthcare startups. To effectively navigate this complex environment, it is essential to develop a thorough understanding of the National Health Service (NHS), the dynamics of private healthcare, the various regulatory frameworks, and the increasing influence of emerging technologies. Each of these elements is integral to aligning your healthcare startup with current industry trends that are destined to shape the future of health services across the United Kingdom.
Exploring the Structure of the NHS and Its Opportunities
The National Health Service serves as the cornerstone of healthcare in the UK, presenting a diverse array of opportunities for innovative startups. Operating on a publicly funded model, the NHS predominantly offers services free at the point of use to residents, which opens numerous avenues for partnerships that can lead to groundbreaking innovations. A comprehensive understanding of the NHS’s structure—comprising various Trusts, Clinical Commissioning Groups (CCGs), and NHS England—is paramount for identifying potential collaboration areas that can enhance service delivery and patient care.
To effectively engage with the NHS, startups must align their services with the priorities outlined in the NHS Long Term Plan, which champions the integration of services, the provision of personalised care, and the embracement of digital technologies. By positioning your solutions in accordance with these strategic objectives, your startup can emerge as a valuable ally in advancing patient care. Additionally, initiatives such as the NHS Innovation and Technology Payment (ITP) programme create pathways for companies to introduce new technologies into the NHS, making it critical to stay updated on sector developments and innovations.
Moreover, the challenges currently faced by the NHS, including staff shortages and rising patient demand, present unique opportunities for startups to deliver innovative solutions. Whether through the development of telehealth platforms, patient management systems, or AI-driven diagnostic tools, understanding these pressing issues can enable your startup to carve out a niche that not only meets the NHS’s needs but also adheres to its operational protocols and standards.
Navigating the Dynamics of Private Healthcare
In addition to the NHS, the private healthcare sector in the UK plays a vital role in shaping the overall healthcare landscape. Private providers cater to patients seeking expedited access to services or specialised treatments that may not be readily available within the NHS framework. For your startup, comprehending the intricacies of private healthcare dynamics is essential for effectively tailoring your offerings to meet market demands.
The emergence of private healthcare facilities, including clinics, hospitals, and diagnostic centres, creates substantial avenues for innovation. Startups can engage with private providers by developing solutions that enhance operational efficiencies or enrich patient experiences. For instance, personalised health tracking apps or platforms that simplify appointment scheduling can resonate well with private providers aiming to attract and retain a loyal clientele.
Furthermore, the COVID-19 pandemic has significantly altered patient perceptions surrounding healthcare, with many individuals now more open to exploring private options. This shift presents a unique opportunity for startups to introduce user-friendly technologies that facilitate seamless access to healthcare services. By aligning your startup’s vision with the evolving expectations of private patients, you can accelerate your entry into the competitive marketplace.
Understanding the Regulatory Landscape
Successfully navigating the regulatory environment is vital for launching a healthcare startup in the UK. The healthcare sector is governed by a myriad of stringent regulations designed to protect patient safety and ensure the delivery of high-quality care. It is crucial for startups to familiarise themselves with organisations such as the Care Quality Commission (CQC) and the Medicines and Healthcare products Regulatory Agency (MHRA) to ensure compliance with industry standards and regulations.
Compliance extends beyond a mere legal obligation; it can also serve as a strategic advantage. A thorough understanding of regulatory frameworks allows startups to build trust with a diverse array of stakeholders, including patients and healthcare providers. For example, startups focusing on digital health solutions must ensure their products meet the rigorous standards established by the General Medical Council (GMC) and adhere to guidelines related to data protection under the General Data Protection Regulation (GDPR).
Moreover, the UK government continually adapts its regulatory landscape to foster innovation. Initiatives like the Digital Health Technology Catalyst are designed to support startups in navigating regulatory challenges while promoting the adoption of groundbreaking solutions. By proactively addressing compliance issues and leveraging these initiatives, your startup can differentiate itself in a competitive healthcare market.
Leveraging Emerging Technologies in Healthcare

The influence of emerging technologies on the UK healthcare sector is profound and transformative. Startups that harness the potential of technologies such as artificial intelligence (AI), telemedicine, and data analytics can greatly enhance service delivery while simultaneously improving patient outcomes across the board.
AI and machine learning stand poised to revolutionise diagnostics and treatment plans. For instance, AI algorithms can analyse extensive datasets to identify disease patterns, enabling earlier diagnoses and more effective treatment strategies. Startups can develop applications that utilise AI for predictive analytics, assisting healthcare providers in making informed decisions based on real-time data insights.
The rise of telemedicine has gained remarkable momentum, particularly during the pandemic, as patients and providers sought safe alternatives to traditional in-person consultations. Startups specialising in telehealth services can effectively bridge the gap between patients and healthcare providers, offering virtual consultations that enhance access to care. This strategic alignment with current trends not only meets patient demand but also positions your startup favourably within the broader healthcare ecosystem.
Additionally, the incorporation of wearable health technology is revolutionising patient monitoring and self-care practices. Startups can explore opportunities to develop devices that empower patients to proactively manage their health. This trend aligns perfectly with the increasing emphasis on personalised care, making it a highly relevant area for innovation. By leveraging these technologies, your startup can effectively position itself at the forefront of the evolving UK healthcare landscape.
The Role of Emerging Technologies in UK Healthcare
As the UK healthcare sector continues to evolve, the integration of emerging technologies represents a crucial pillar of transformation. Startups that successfully tap into these advancements can not only enhance their service offerings but also play a significant role in shaping the future of healthcare delivery.
Expanding Telemedicine and Remote Care Solutions
Telemedicine has surged in popularity, driven by the urgent need for accessible healthcare during the pandemic. This trend has reinforced the role of remote care as a legitimate alternative to conventional healthcare models. Startups entering this domain can capitalise on the growing demand for innovative solutions that allow for seamless patient-provider interactions.
The convenience offered by telemedicine cannot be overstated. Patients can consult healthcare professionals from the comfort of their own homes, effectively minimising the barriers associated with travel and long wait times. For your startup, developing a robust telemedicine platform that prioritises user experience can significantly enhance patient satisfaction levels. Features such as secure messaging, video consultations, and simplified appointment scheduling could differentiate your solution from competitors in the marketplace.
Moreover, integrating telemedicine into primary care settings can alleviate pressures on the NHS by enabling providers to triage patients more effectively. Startups can explore partnerships with GP practices and NHS Trusts to create customised telehealth solutions tailored to diverse patient populations. This approach maximises the effectiveness of healthcare delivery and aligns your startup with the broader objectives of the UK healthcare system.
As remote care continues to gain traction, investing in patient education about the benefits of telemedicine is of paramount importance. Your startup should create informative materials that guide patients on how to optimise their telehealth experiences, thus fostering greater engagement and encouraging wider adoption of such services.
Innovating with AI and Machine Learning Technologies
Artificial intelligence and machine learning are increasingly being acknowledged as transformative forces in the healthcare landscape. By automating processes and analysing data on an unprecedented scale, these technologies offer a pathway to enhance the quality of care while optimising operational efficiencies.
Startups can explore a wide array of applications for AI within healthcare, from predictive analytics that identify at-risk patients to natural language processing tools that streamline administrative workflows. For example, AI algorithms could scrutinise patient data to flag potential health risks before they escalate, enabling proactive intervention and improving patient outcomes.
One notable advantage of machine learning lies in its capacity to process vast amounts of data, which is particularly beneficial in the realms of genomics and personalised medicine. Startups that develop solutions focusing on precision medicine can position themselves as pioneers in a rapidly expanding market. By employing AI to tailor treatment plans based on individual patient profiles, your startup can contribute to delivering more effective and targeted healthcare solutions.
To fully leverage AI technologies, startups should consider forming collaborations with academic institutions and research centres. These partnerships can offer access to expertise and datasets, fostering innovation while ensuring alignment with the latest advancements in the healthcare field. In doing so, your startup can establish a reputation as a forward-thinking entity within the healthcare ecosystem.
Revolutionising Health Monitoring with Wearable Technology
The proliferation of wearable health technology has significantly transformed how individuals monitor and manage their health. Devices such as fitness trackers, smartwatches, and health monitors are gaining popularity, providing a wealth of opportunities for startups looking to engage with this burgeoning trend.
Wearable technology empowers patients to take an active role in their health management. For instance, devices that track heart rate, activity levels, and sleep patterns can furnish individuals with valuable insights into their overall wellbeing. Startups can capitalise on this trend by developing applications that interpret data collected from wearables, offering personalised recommendations based on users’ health statuses.
Furthermore, the integration of wearables into healthcare systems can lead to improved patient outcomes. Startups that devise solutions enabling seamless data sharing between patients and healthcare providers can enhance communication and continuity of care. This alignment with the UK health service’s focus on integrated care significantly bolsters your startup’s value proposition.
As demand for wearable technology continues to rise, it is essential for startups to consider the ethical implications surrounding data privacy and security. Ensuring that user data is protected and utilised responsibly will not only foster trust but also ensure compliance with regulatory standards, thereby reinforcing your startup’s credibility in the marketplace.
Blockchain Technology in Healthcare Data Management
Blockchain technology is increasingly being recognised for its potential to revolutionise data management within the healthcare sector. With its decentralised and secure architecture, blockchain presents solutions to the pressing challenges of data interoperability and security within the UK’s healthcare framework.
Startups can explore opportunities to leverage blockchain for secure patient data management. By creating platforms that utilise blockchain technology, your startup can offer healthcare providers a secure means to share patient information while maintaining control over data access. This innovation can enhance data integrity, reduce errors, and improve patient outcomes significantly.
Moreover, blockchain can play a pivotal role in enhancing the transparency of clinical trials and pharmaceutical supply chains. Startups focusing on developing blockchain solutions for tracking the provenance of medications can substantially contribute to patient safety while addressing concerns related to counterfeit drugs.
In the NHS context, integrating blockchain technology could streamline administrative processes such as billing and claims management. By minimising paperwork and improving data accuracy, your startup can help reduce some of the administrative burdens faced by healthcare providers, positioning itself as an essential partner in driving efficiency.
As the UK healthcare sector continues to advance, remaining informed about technological advancements will be crucial for your startup’s success. By leveraging blockchain, your healthcare solution can not only enhance operational efficiencies but also ensure compliance with regulatory standards, thereby solidifying your startup’s standing within the market.
Exploring Funding and Investment Opportunities
Securing funding and investment is a vital aspect of launching and scaling a healthcare startup in the UK. The landscape brims with opportunities, ranging from government grants to private investment channels, all of which can empower your venture to flourish in a competitive market environment.
Accessing Government Grants and Initiatives
The UK government has implemented various grants and initiatives aimed at promoting innovation within the healthcare sector. Startups should actively pursue funding opportunities provided by agencies such as Innovate UK, which offers grant funding for projects demonstrating strong growth potential and societal impact.
A clear understanding of the eligibility criteria for these grants is essential for crafting compelling applications. Startups must effectively articulate how their solutions align with national healthcare priorities, such as enhancing patient outcomes or improving efficiency within the NHS. By positioning your startup as a contributor to these overarching goals, you increase your chances of successfully securing funding.
Additionally, the NHS has introduced several funding initiatives, including the NHS Innovation Accelerator programme, which supports the scaling of innovations within the NHS. Startups that can showcase their potential to drive positive transformation in healthcare delivery are well-positioned to reap the benefits of these initiatives.
Furthermore, local councils and health authorities often maintain their own innovation funds, encouraging startups to engage with these entities in promoting local healthcare solutions. By actively seeking out these funding opportunities, your startup can secure crucial financial backing while reinforcing its commitment to enhancing health services within the community.
Engaging with Venture Capital and Angel Investors
Venture capital (VC) and angel investors play a critical role in funding healthcare startups, providing not only financial resources but also invaluable mentorship and industry connections. The UK boasts a vibrant investment ecosystem, with numerous VC firms focusing specifically on healthcare innovations.
To attract the right investors, startups should develop a well-structured business plan that outlines their value proposition, market potential, and revenue model. Emphasising how your startup’s innovations align with current healthcare trends can generate interest among potential investors seeking impactful opportunities.
Networking is essential when pursuing investment. Attending industry conferences, pitch events, and startup competitions can offer opportunities to connect with investors actively looking to support healthcare innovations. Engaging with industry-specific networks, such as the UK HealthTech Network, also enhances visibility and increases the likelihood of securing investment.
Moreover, UK-based angel investor networks, such as Angel Investment Network and Seedrs, provide platforms for startups to showcase their innovations and seek funding. Crafting a compelling pitch that highlights your startup’s impact on patient care can resonate well with investors seeking meaningful investment opportunities.
Utilising Crowdfunding and Alternative Financing Options
Crowdfunding has emerged as an innovative method for healthcare startups to raise capital while simultaneously building a community of supporters around their products and services. Platforms like Crowdcube and Kickstarter allow startups to reach a broad audience, making it easier to secure funding for innovative healthcare solutions.
By employing engaging storytelling and visually appealing content, your startup can attract potential investors who resonate with your mission and vision. Crowdfunding also provides an opportunity to gauge market interest before fully launching your product, offering valuable insights into customer preferences and demand.
In addition to crowdfunding, exploring alternative financing options such as peer-to-peer lending and grants from charitable foundations can provide supplementary funding sources. Engaging with financial advisors who specialise in healthcare startups can help identify the most effective strategies for financing your venture.
Furthermore, social impact investors are increasingly seeking opportunities to invest in companies that demonstrate a commitment to improving healthcare outcomes. By aligning your startup’s mission with their values, you can tap into this growing segment of financiers eager to support health-related initiatives.
Forging Strategic Partnerships and Collaborations
Establishing strategic partnerships and collaborations can significantly enhance your healthcare startup’s access to funding and resources. By aligning with established healthcare organisations, startups can leverage their networks, expertise, and market presence to accelerate growth and innovation.
Identifying potential partners within the NHS, private healthcare providers, or academic institutions can yield fruitful collaborations. For instance, partnering with an NHS Trust can provide access to valuable insights and data, enabling your startup to tailor its solutions to meet the specific needs of healthcare providers and patients alike.
Collaborations can also facilitate joint funding applications, pooling resources and expertise to tackle common challenges within the healthcare sector. This approach not only enhances your startup’s credibility but also broadens its reach and influence within the healthcare ecosystem.
Moreover, engaging with healthcare incubators and accelerators can foster strategic partnerships. These programmes often connect startups with industry leaders and provide mentorship, funding opportunities, and invaluable networking. Startups that participate in these initiatives can gain insights into market trends while refining their business models and strategies for success.
By actively pursuing partnerships and collaborations, your healthcare startup can secure the support and resources necessary to thrive in the competitive landscape of the UK market.
The Role of Incubators and Accelerators
Incubators and accelerators play a crucial role in nurturing healthcare startups by providing essential funding, mentorship, and networking opportunities. The UK is home to several healthcare-focused incubators, each offering unique resources designed to help startups navigate the complexities of scaling their ventures.
Participating in an incubator can grant early-stage startups access to critical resources, including office space, technical support, and business development guidance. Programmes like the DigitalHealth.London Accelerator specifically target health tech startups, providing tailored mentorship and access to NHS experts who can guide your venture’s growth.
Moreover, incubators often facilitate connections with potential investors and stakeholders, providing startups with a platform to showcase their innovations. This exposure can be invaluable for attracting funding and forming strategic partnerships, ensuring that your startup is well-positioned for future growth.
Accelerators typically offer structured programmes culminating in pitch days, where startups present their solutions to panels of investors. This format not only helps refine your pitch but also provides a direct avenue for securing funding. Engaging with these programmes can significantly enhance your startup’s visibility within the healthcare landscape.
Additionally, incubators often encourage collaboration among startups, fostering an environment of shared learning and innovation. By participating in these ecosystems, your healthcare startup can benefit from the collective expertise and experiences of fellow innovators, ultimately driving your growth and success.
Building Collaborations and Partnerships
Collaborations and partnerships are crucial for healthcare startups aiming to thrive in the competitive UK market. By establishing strategic alliances with academic institutions, industry networks, and public sector entities, startups can enhance their innovation capabilities, broaden their reach, and ultimately improve patient outcomes.
Partnering with Academic and Research Institutions
Collaborating with academic and research institutions can provide healthcare startups with access to cutting-edge research, expertise, and invaluable resources. Renowned UK universities such as Oxford and Cambridge are celebrated for their contributions to medical research and innovation, making them ideal partners for startups seeking to develop new healthcare solutions.
By engaging with researchers and faculty members, your startup can leverage their knowledge and experience to refine product offerings. For instance, partnering with a university can facilitate clinical trials, enabling your startup to validate its solutions within real-world settings. This not only enhances your credibility but also provides essential data to support funding applications and regulatory approvals.
Moreover, academic institutions often have established networks within the healthcare sector, offering valuable connections to potential customers and stakeholders. By collaborating with these entities, your startup can enhance its visibility and establish itself as a thought leader in the field.
Furthermore, many universities offer innovation hubs or incubators that provide dedicated support for startups. Joining these programmes can offer access to funding opportunities, mentorship, and resources, bolstering your startup’s growth trajectory and innovative capabilities.
Joining Industry Alliances and Networks
Becoming part of industry alliances and networks can significantly enhance your healthcare startup’s visibility and collaboration prospects. The UK boasts numerous organisations dedicated to fostering innovation and collaboration within the healthcare sector, such as the UK HealthTech Alliance and the Digital Health Innovation Network.
These alliances provide a platform for startups to connect with key stakeholders, including healthcare providers, investors, and policymakers. By actively participating in industry events, workshops, and networking sessions, your startup can establish relationships that may lead to strategic partnerships and collaborations.
Additionally, being part of an industry alliance enhances your startup’s credibility and reputation within the sector. These organisations often advocate for policy changes and funding opportunities that benefit their members, providing an additional layer of support for your venture.
Moreover, industry networks can facilitate knowledge sharing and collaboration among startups facing similar challenges. By engaging with peers, your startup can gain insights into best practices, emerging trends, and innovative solutions, ultimately driving your growth and innovation potential.
Collaborations with the NHS and Public Sector Entities
Forging partnerships with the NHS and other public sector entities can significantly propel your healthcare startup’s growth trajectory. The NHS actively seeks innovative solutions to address its challenges, making it an ideal partner for startups aiming to make a meaningful impact.
Engaging with NHS Trusts and Clinical Commissioning Groups (CCGs) can provide startups with valuable insights into the specific needs and priorities of healthcare providers. By tailoring your solutions to align with NHS goals, your startup can position itself as a valuable contributor to the overall healthcare ecosystem.
Additionally, partnerships with public sector entities can facilitate access to funding opportunities, such as government grants and innovation challenges. By demonstrating how your startup addresses the pressing needs of the NHS, you can secure essential resources to support your growth and development.
Furthermore, collaborating with the NHS can enhance your startup’s credibility, as association with a respected public health institution can foster trust with patients and healthcare providers alike. This trust can be instrumental in driving the adoption of your solutions within the healthcare sector.
To maximise the benefits of public sector partnerships, startups should proactively seek collaboration opportunities, whether through pilot projects, joint research initiatives, or technology integration efforts. By doing so, your healthcare startup can thrive in the dynamic UK market.
Fostering Patient-Centric Innovations
In today’s healthcare landscape, adopting a patient-centric approach is essential for startups aspiring to create a meaningful impact. By focusing on personalised medicine, patient engagement, and mental health initiatives, your healthcare startup can enhance its value proposition while addressing the evolving needs of UK patients.
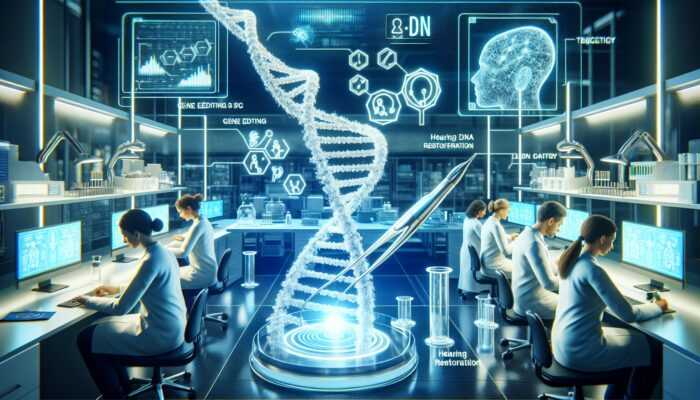
Advancing Personalised Medicine Approaches
Personalised medicine represents a paradigm shift in healthcare, enabling tailored treatment plans based on an individual’s unique genetic makeup, lifestyle, and preferences. Startups that harness the power of personalised medicine can significantly enhance patient care while differentiating themselves in a competitive market landscape.
Developing solutions that incorporate genetic and biomarker data can empower healthcare providers to deliver more effective treatments. For example, startups can create platforms that analyse genetic information to identify patients most likely to benefit from specific therapies. This not only improves treatment efficacy but also minimises trial-and-error approaches, ultimately enhancing patient outcomes.
Moreover, personalised medicine aligns well with the growing demand for patient empowerment. By providing patients with insights into their health and treatment options, startups can foster greater engagement and adherence to treatment plans. Educational resources and tools that empower patients to actively participate in their care can strengthen your startup’s value proposition in the healthcare market.
Collaboration with academic institutions and research centres can further bolster your efforts in personalised medicine. By partnering with experts in genomics and bioinformatics, your startup can stay at the forefront of advancements in the field, ensuring that your solutions remain relevant and impactful in the evolving healthcare landscape.
Enhancing Patient Engagement and Education
Engaging and educating patients is critical for driving the adoption of healthcare solutions. Startups should develop strategies that facilitate communication and ensure that patients understand the benefits of their offerings. This could include creating user-friendly platforms that provide educational content, resources, and support tailored to patient needs.
Utilising digital channels such as social media, blogs, and webinars can significantly enhance patient engagement. By sharing success stories, informative articles, and interactive content, your startup can cultivate a community of informed patients who are more likely to engage with and utilise your solutions.
Additionally, incorporating feedback mechanisms can help startups understand patient needs and preferences more effectively. Surveys, focus groups, and user testing can provide valuable insights that inform product development and enhance user experiences. By actively listening to patients, your startup can continuously refine its offerings to align with evolving expectations and demands.
Furthermore, forging partnerships with healthcare providers can facilitate educational initiatives. Collaborating with doctors and nurses can enhance the credibility of your startup’s messaging while ensuring that patients receive accurate information about available solutions and treatment options.
Prioritising Mental Health and Wellbeing
The growing demand for mental health and wellbeing services presents substantial opportunities for healthcare startups. With increasing awareness of mental health issues, patients are actively seeking innovative solutions to support their mental and emotional wellbeing.
Startups can develop digital platforms that offer resources for mental health support, including therapy apps, mindfulness tools, and community forums. By providing easy access to mental health services, your startup can effectively address the challenges faced by individuals seeking support and guidance.
Moreover, integrating mental health services into primary care settings can enhance access and reduce stigma. Collaborating with NHS services to offer integrated mental health solutions can position your startup as a leader in addressing this pressing need within the healthcare sector.
Additionally, partnerships with established mental health organisations can bolster your startup’s credibility and reach. By aligning your mission with respected entities in the mental health space, you can leverage their expertise and networks to drive awareness and adoption of your solutions.
The focus on mental health and wellbeing aligns with the broader movement towards holistic healthcare, ensuring that your startup remains relevant and impactful in a rapidly changing landscape.
Ensuring Data Privacy and Security
In the digital age, prioritising data privacy and security is paramount for healthcare startups navigating the UK healthcare landscape. With increasing scrutiny and regulatory requirements, safeguarding data protection not only builds trust but also reinforces your startup’s credibility within the sector.
Ensuring GDPR Compliance in Healthcare
Compliance with the General Data Protection Regulation (GDPR) is essential for all healthcare startups operating in the UK. GDPR establishes stringent standards for how personal data is collected, processed, and stored, making it imperative for startups to ensure that their practices conform to these regulations.
Startups should conduct comprehensive assessments of their data management practices to identify areas for improvement. This includes implementing robust policies, obtaining informed consent from patients, and ensuring that data is securely stored and accessed only by authorised personnel.
Moreover, transparency is vital in building trust with patients. Startups should clearly communicate how patient data will be used and protected, fostering a culture of openness that encourages patients to engage with their services. By prioritising GDPR compliance, your startup can establish itself as a responsible and trustworthy entity within the healthcare landscape.
Additionally, incorporating privacy by design principles into your product development process can enhance compliance. By embedding data protection measures from the outset, your startup can mitigate risks and ensure that patient privacy remains a top priority throughout the development lifecycle.
Implementing Robust Cybersecurity Measures
Cybersecurity is a critical concern for healthcare startups, given the sensitive nature of patient data. Implementing robust cybersecurity measures is essential to safeguard against data breaches and cyber-attacks that could compromise patient information and trust.
Startups should invest in advanced security technologies, such as encryption, firewalls, and intrusion detection systems. Regular security audits and vulnerability assessments can help identify potential weaknesses and ensure that your startup’s systems remain secure against evolving threats.
Moreover, employee training is crucial in fostering a culture of cybersecurity awareness. Staff should be educated on best practices for data protection, including recognising phishing attempts and securely handling patient information. By prioritising cybersecurity, your startup can effectively mitigate risks and protect sensitive patient data.
Additionally, developing an incident response plan can prepare your startup to respond swiftly and effectively to potential security incidents. This proactive approach can minimise the impact of cyber threats and reinforce patient confidence in your startup’s commitment to data protection and privacy.
Promoting Ethical Data Use and Transparency
Promoting ethical data use and transparency is essential for building trust with patients and stakeholders in the healthcare sector. Startups should establish clear guidelines for how patient data will be utilised, ensuring that it aligns with ethical principles and supports patient wellbeing.
Engaging with patients in discussions about data usage can foster a sense of empowerment and ownership over their information. By involving patients in decision-making processes, your startup can enhance transparency and build stronger relationships with your audience, ultimately driving engagement and adoption.
Furthermore, considering the ethical implications of data-driven innovations is crucial. Startups should assess how their solutions may impact patient privacy and autonomy, ensuring that ethical considerations are prioritised throughout the development process to avoid potential pitfalls.
By championing ethical data use and transparency, your healthcare startup can position itself as a responsible and trustworthy entity in the rapidly evolving landscape, ultimately enhancing patient trust and satisfaction.
Implementing Effective Data Encryption Techniques
Data encryption is a fundamental aspect of safeguarding patient information within healthcare startups. Implementing advanced encryption techniques can protect sensitive data from unauthorised access, ensuring that patient confidentiality is upheld at all times.
Startups should adopt industry-standard encryption protocols for data both at rest and in transit. By encrypting sensitive patient information, your startup can mitigate the risks associated with data breaches and cyber threats, thereby reinforcing your commitment to data protection and patient privacy.
Moreover, integrating encryption methods into your products and services can enhance compliance with regulatory requirements, such as GDPR. By prioritising encryption, your startup demonstrates a proactive approach to safeguarding patient data, which can significantly enhance trust and credibility within the healthcare sector.
Additionally, regular assessments of encryption practices are essential to ensure they remain effective against evolving threats. Staying informed about the latest encryption technologies and best practices can help your startup maintain a robust security posture and protect patient information effectively.
Conducting Regular Data Audits and Monitoring
Conducting regular data audits and monitoring is critical for ensuring ongoing compliance and security within healthcare startups. These practices help identify potential vulnerabilities and ensure that data management processes remain aligned with regulatory requirements and best practices.
Startups should establish a routine for auditing data management practices, evaluating the effectiveness of security measures, and identifying areas for improvement. This proactive approach can help mitigate risks and ensure that patient data is protected effectively.
Moreover, implementing monitoring systems can provide real-time visibility into data access and usage. By tracking who accesses patient information and how it is used, your startup can identify potential breaches or misuse early, allowing for swift corrective actions to mitigate risks.
Additionally, documenting audit and monitoring processes can enhance accountability and transparency. By maintaining thorough records of data management practices, your startup can demonstrate its commitment to compliance and data protection, thereby reinforcing trust among patients and stakeholders.
Through regular audits and monitoring, healthcare startups can build a culture of accountability and trust, ultimately enhancing patient confidence in their products and services.
Workforce Development and Talent Acquisition Strategies
Developing a skilled workforce is vital for healthcare startups aiming to succeed in the dynamic UK market. Identifying the specific skills and training needs of your team can enhance competitiveness while ensuring that your startup is well-equipped to address the challenges inherent in the healthcare sector.
Identifying Skills and Training Needs
The rapidly evolving landscape of healthcare technology demands a workforce with diverse skills and competencies. Startups should assess their current team’s capabilities and identify gaps that may hinder growth and innovation.
Key areas of focus should include technical skills, data analytics, and knowledge of regulatory compliance. As healthcare increasingly relies on data-driven decision-making, equipping your team with data analytics skills can enhance their ability to derive insights and drive improvements in patient care.
Additionally, investing in ongoing training and professional development is essential for fostering a culture of innovation within your startup. Providing access to workshops, courses, and industry conferences can empower your team to stay abreast of the latest trends and technologies, ultimately driving your startup’s competitive edge in the healthcare market.
Moreover, fostering a collaborative and inclusive workplace culture can enhance employee satisfaction and retention. Encouraging open communication and teamwork can stimulate creativity and innovation, leading to the development of transformative healthcare solutions that address pressing patient needs.
By prioritising workforce development and training, your healthcare startup can build a talented and motivated team, ensuring that you remain agile and responsive in an ever-changing landscape while driving meaningful impact in the healthcare sector.
Frequently Asked Questions (FAQs)
What are the key trends shaping UK healthcare startups?
Key trends include the growing adoption of telemedicine, AI-driven healthcare solutions, personalised medicine approaches, and the integration of wearable technology for patient monitoring and engagement.
How can my startup establish partnerships with the NHS?
Startups can engage with the NHS through innovation programmes, pilot projects, and collaborative efforts aimed at addressing specific healthcare challenges and improving patient outcomes across the system.
What funding options are available for healthcare startups in the UK?
Funding options include government grants, venture capital, angel investors, crowdfunding, and strategic partnerships with established healthcare organisations that can provide financial backing and resources.
How can I ensure compliance with GDPR regulations for my healthcare startup?
Ensure compliance by implementing comprehensive data protection policies, obtaining informed consent from patients, and conducting regular audits of your data management practices to align with regulatory requirements.
What role does technology play in enhancing patient engagement?
Technology enhances patient engagement by providing easy access to information, streamlining communication channels, and enabling personalised care through digital platforms and applications.
How can my startup focus on developing mental health solutions?
Develop digital platforms that offer mental health resources, therapy options, and community support programs, addressing the growing demand for mental health services in the UK healthcare landscape.
What are effective strategies for educating patients about healthcare solutions?
Effective strategies include creating user-friendly educational resources, utilising digital channels for outreach, and collaborating with healthcare providers to disseminate accurate information about available solutions and treatments.
How can startups leverage emerging technologies to improve healthcare delivery?
Startups can leverage emerging technologies such as AI, telemedicine, and blockchain to enhance service delivery, improve patient outcomes, and streamline operations within healthcare systems.
What are the benefits of establishing strategic partnerships in healthcare?
Strategic partnerships can provide access to funding, expertise, resources, and networks, enhancing your startup’s credibility and market presence while facilitating innovation and growth.
Why is workforce development critical for healthcare startups?
Workforce development ensures that your team possesses the necessary skills to navigate challenges, drive innovation, and maintain competitiveness in the evolving healthcare landscape, ultimately contributing to your startup’s success.
The post Aligning Healthcare Startups with Current Industry Trends appeared first on Healthcare Marketing Service.