Complying with Healthcare Vendor Contracts: Essential Guide
Comprehensive Guide to UK Healthcare Regulations and Vendor Management
Adhering to NHS Standards for Quality Care
The National Health Service (NHS) operates within a rigorous framework of standards that governs interactions between healthcare providers and their vendors. Adhering to these standards is crucial, as they ensure that vendors furnish high-quality services that align with public health objectives. The NHS standards cover various domains, including patient safety, effectiveness, and patient experience. Vendors need to fully grasp these standards and their applicability to their services, particularly concerning procurement procedures and service delivery.
When engaging with healthcare vendors, NHS organisations must ensure that contracts explicitly stipulate adherence to these standards. This includes outlining service specifications that detail the expected quality and outcomes from the vendor’s offerings. Conducting regular reviews and audits of service delivery against these standards is paramount, as they provide accountability and protect patient interests. By committing to these standards, NHS entities can significantly reduce risks associated with vendor non-compliance, placing patient care at the forefront of every contractual agreement.
Furthermore, compliance with NHS standards promotes a culture of transparency and trust—vital components in the healthcare sector. Vendors who align their operations with NHS standards exhibit a commitment to quality and patient wellbeing. This alignment can also bolster their reputation, leading to more partnerships and opportunities within the UK healthcare ecosystem. Ultimately, understanding and complying with NHS standards transcends regulatory requirements; it embodies a moral obligation that benefits all stakeholders involved in healthcare delivery.
Essential Care Quality Commission (CQC) Guidelines for Vendors
The Care Quality Commission (CQC) plays a pivotal role in regulating and monitoring healthcare services across the UK, including the compliance of healthcare vendors. The CQC establishes critical guidelines that ensure service providers deliver high-quality care, shaping the contractual landscape for healthcare vendors. For organisations aiming to comply with healthcare vendor contracts, a robust understanding of CQC guidelines is indispensable.
These guidelines focus on five fundamental areas: safety, effectiveness, caring, responsiveness, and well-led services. Vendors must substantiate their capacity to meet these standards, typically evaluated through inspections and ongoing monitoring. Contracts with healthcare vendors should explicitly mandate compliance with CQC guidelines, incorporating mechanisms for accountability and performance evaluation.
To align vendor operations with CQC standards, healthcare organisations ought to conduct regular assessments and audits, ensuring that vendors remain compliant. Establishing performance metrics closely tied to CQC outcomes is a proactive approach to addressing potential issues while cultivating a culture of continuous improvement among vendors.
Understanding the ramifications of CQC guidelines on vendor contracts not only facilitates regulatory compliance but also bolsters the overarching mission of delivering safe and effective patient care. Vendors who align with these guidelines are more likely to forge enduring partnerships that significantly enhance the quality of care offered to patients within the NHS framework.
Data Protection Act Compliance for Healthcare Vendors
The Data Protection Act (DPA) is a cornerstone of regulatory compliance in the UK, particularly concerning healthcare vendors. This legislation governs the management of personal data, providing robust protections for patient information. For healthcare organisations, ensuring that vendors adhere to the DPA is critical, as breaches can lead to severe penalties and reputational harm.
Healthcare vendors are required to implement stringent data security measures to protect personal and sensitive information. Contracts should explicitly stipulate compliance with the DPA, detailing the vendor’s responsibilities related to data handling, storage, and sharing. This encompasses the need for robust encryption methods, secure data transfer protocols, and clear guidelines for data retention and disposal.
Moreover, healthcare organisations should maintain oversight by conducting regular audits and evaluations of vendor data protection practices. This ensures adherence to the DPA while identifying potential vulnerabilities that could jeopardise patient data security. By fostering a culture of data protection within vendor relationships, organisations can significantly mitigate the risk of data breaches and enhance patient trust.
Incorporating DPA principles into vendor contracts is not merely a regulatory obligation; it is a vital step in safeguarding patient privacy and upholding the integrity of the healthcare system. By prioritising data protection, healthcare organisations can effectively navigate the complexities of vendor relationships while ensuring compliance and protecting patient rights.
Navigating the Health and Social Care Act
The Health and Social Care Act lays down a robust regulatory framework governing healthcare services in the UK, profoundly influencing vendor contracts. This legislation aims to foster integrated care and enhance service quality, directly impacting how healthcare providers engage with vendors. Understanding the implications of this Act is critical for organisations seeking compliance with healthcare vendor contracts.
Under the Health and Social Care Act, healthcare providers are mandated to collaborate effectively with vendors to facilitate seamless service delivery. Contracts must embody this collaborative spirit, explicitly detailing the expectations for service integration and quality outcomes. By nurturing partnerships that align with the principles of the Act, healthcare organisations can significantly enhance service delivery and improve patient experiences.
Additionally, the Act underscores the significance of accountability and transparency in service provision. Vendors must be prepared to demonstrate their compliance with regulatory standards, as failure to do so may result in severe consequences for both the vendor and the healthcare provider. Regular performance reviews coupled with transparent communication channels are vital for maintaining compliance and ensuring that vendor services meet the expectations set forth in the legislation.
Incorporating the Health and Social Care Act into vendor contracts promotes a holistic approach to patient care, ensuring all parties are united in their commitment to delivering quality services. This alignment not only fortifies compliance but also strengthens the relationships between healthcare providers and vendors, ultimately benefiting patient outcomes.
Understanding the Mental Health Act in Vendor Relationships
The Mental Health Act governs the treatment and care of individuals with mental health conditions in the UK, imposing specific requirements that impact healthcare vendor contracts. For organisations operating within the mental health sector, comprehending the implications of this Act is vital for ensuring compliance and safeguarding patient rights.
Vendor contracts must reflect the provisions of the Mental Health Act, detailing the expected standards of care in treating patients with mental health issues. This includes stipulations around capacity assessments, patient consent, and the provision of suitable safeguarding measures. Vendors must not only comply with the Act but also demonstrate a steadfast commitment to upholding the dignity and rights of patients.
Regular training and education for vendors concerning the Mental Health Act is essential for maintaining compliance. This might involve organising workshops and awareness programmes focused on the intricacies of the Act and its practical implications for service delivery. By prioritising mental health training, healthcare organisations can cultivate a well-informed vendor workforce capable of addressing the unique needs of this patient demographic.
Furthermore, establishing clear channels for reporting and addressing concerns related to mental health care is crucial. Contracts should incorporate mechanisms for feedback and accountability, enabling healthcare organisations to effectively monitor vendor compliance with the Mental Health Act. By embedding these practices within vendor relationships, organisations can promote a culture of excellence in mental health care, ultimately enhancing patient outcomes and experiences.
Critical Elements of UK Vendor Contracts
Establishing Effective Service Level Agreements (SLAs)
In the realm of healthcare vendor contracts, Service Level Agreements (SLAs) are indispensable tools for ensuring quality and accountability. These agreements delineate the specific services a vendor is obliged to provide and establish performance standards. By articulating expectations clearly, SLAs create a framework within which vendors must operate, empowering healthcare organisations to hold them accountable for their commitments.
SLA components typically comprise performance metrics, response times, and service quality standards. For instance, a healthcare organisation may specify that a vendor must respond to service requests within a designated timeframe or maintain a certain satisfaction rating from patients. These metrics not only provide benchmarks for performance but also empower organisations to systematically assess vendor effectiveness.
Regular reviews of SLAs are crucial to ensure they remain relevant and aligned with organisational objectives. As healthcare needs evolve, so too must the agreements governing vendor relationships. By integrating feedback mechanisms and performance evaluations into SLAs, organisations can cultivate an environment of continuous improvement that enhances both vendor performance and patient care outcomes.
Moreover, effective communication regarding SLAs is paramount. Healthcare organisations should engage vendors in discussions about performance expectations and any potential challenges they may encounter in meeting these standards. This collaborative approach not only strengthens vendor relationships but also fosters a shared commitment to achieving exceptional patient care.
In essence, well-structured SLAs serve as the foundation for successful healthcare vendor contracts. By prioritising these agreements, organisations can mitigate risks and ensure that vendors deliver the quality of service required to meet the needs of patients and the healthcare system as a whole.
Defining Clear Termination Clauses
Termination clauses represent a critical aspect of healthcare vendor contracts, providing a clear framework for ending the relationship when necessary. These clauses protect both parties by stipulating the conditions under which a contract may be terminated, ensuring that the process is conducted efficiently and transparently.
In the context of healthcare, termination implications can be significant. For instance, if a vendor consistently fails to meet performance expectations or breaches critical compliance requirements, having a well-defined termination clause empowers healthcare organisations to take decisive action. This not only safeguards the organisation’s interests but also protects patient care, enabling a swift transition to a more suitable vendor if necessary.
Termination clauses should include specific provisions regarding notice periods, grounds for termination, and the obligations of both parties during the termination process. Such clarity minimizes confusion and potential disputes, ensuring that all parties comprehend their rights and responsibilities.
Moreover, organisations must consider the implications of termination on ongoing patient care. Contracts should outline protocols for ensuring continuity of care, thereby minimizing disruption to patients during vendor transitions. This might involve planning for handover procedures or identifying interim solutions to maintain service levels.
Ultimately, termination clauses serve as safeguards for healthcare organisations, ensuring they have the flexibility to address challenges in vendor performance. By embedding these clauses in vendor contracts, organisations can proactively manage relationships, protecting both their interests and the quality of patient care.
Ensuring Confidentiality Agreements Are in Place
Confidentiality agreements play a fundamental role in healthcare vendor contracts, safeguarding sensitive patient information and ensuring compliance with data protection regulations. These agreements establish clear expectations regarding the handling of confidential data, which is particularly crucial given the vulnerabilities associated with sharing patient information.
Healthcare vendors often have access to a wealth of sensitive data, ranging from medical histories to treatment plans. As such, confidentiality agreements must outline the specific obligations of vendors in protecting this information. This includes stipulations concerning data storage, access controls, and protocols for information sharing, ensuring that vendors implement robust security measures to prevent data breaches.
Moreover, confidentiality agreements should incorporate provisions for ongoing training and awareness, ensuring that all vendor employees comprehend the importance of data protection. Regular training sessions focused on confidentiality best practices can empower vendors to safeguard information effectively, thereby minimising the risk of accidental disclosures.
Monitoring compliance with confidentiality agreements is equally important. Healthcare organisations should establish protocols for auditing vendor practices, ensuring adherence to the terms outlined in the agreement. This may involve regular assessments of vendor data security measures and feedback mechanisms for reporting potential breaches.
Incorporating confidentiality agreements into healthcare vendor contracts is not merely a regulatory requirement; it is a moral imperative. By prioritising patient privacy and data protection, organisations can foster trust and confidence among patients, reinforcing their commitment to safeguarding sensitive information throughout the vendor relationship.
Liability and Indemnity Provisions for Protection
Liability and indemnity provisions are integral components of healthcare vendor contracts, establishing the responsibilities of each party in the event of loss, damage, or legal claims. These provisions outline the extent to which vendors are accountable for any harm that may arise from their services, shielding healthcare organisations from potential liabilities.
In the healthcare sector, the implications of liability can be profound. Vendors must ensure they carry adequate insurance coverage to meet the demands of these contractual obligations. This includes coverage for claims related to professional negligence, data breaches, or adverse incidents linked to their services.
Indemnity provisions further protect healthcare organisations by obligating vendors to compensate them for any losses incurred due to vendor negligence or contractual breaches. These provisions must be clearly articulated in the contract to avoid ambiguity and potential disputes. By establishing clear lines of responsibility, organisations can mitigate risks associated with vendor relationships, ensuring they are financially protected in unforeseen circumstances.
Moreover, healthcare organisations should regularly review and update liability and indemnity provisions in vendor contracts to reflect changes in legislation or industry standards. This proactive approach ensures that contracts remain robust and suitable in an evolving regulatory landscape.
Ultimately, well-defined liability and indemnity provisions are essential for safeguarding healthcare organisations and maintaining the integrity of patient care. By prioritising these components in vendor contracts, organisations can confidently navigate the complexities of vendor relationships, ensuring they are prepared for any potential challenges that may arise.
Data Protection Compliance in Vendor Contracts
In today’s digital landscape, data protection compliance has become a cornerstone of healthcare vendor contracts, particularly in light of stringent regulations such as the General Data Protection Regulation (GDPR). Ensuring that vendors comply with these regulations is vital for safeguarding patient information and maintaining trust within the healthcare system.
Vendor contracts must explicitly require compliance with data protection laws, outlining the obligations vendors have regarding the collection, processing, and storage of personal data. This includes ensuring that vendors implement appropriate security measures to protect data from breaches or unauthorised access. Specific clauses may detail encryption standards, access controls, and incident response protocols to mitigate risks effectively.
Additionally, healthcare organisations should conduct thorough due diligence before engaging with vendors, assessing their data protection practices and history. This might involve reviewing compliance certifications or conducting audits to ensure they meet necessary standards. Establishing a clear framework for monitoring vendor compliance throughout the contract’s duration is equally important, as it helps identify potential vulnerabilities and address them promptly.
Education and training regarding data protection compliance are essential for vendors. Healthcare organisations should provide resources and support to ensure vendor staff understands their obligations under data protection laws. This commitment to ongoing education fosters a culture of compliance, enhancing the overall quality of service delivery.
By prioritising data protection compliance in vendor contracts, healthcare organisations can navigate the complexities of regulatory requirements while safeguarding patient information. This focus not only protects against potential legal repercussions but also reinforces the commitment to maintaining trust and integrity within the healthcare system.
Monitoring Compliance and Reporting Mechanisms
Implementing Regular Audits for Compliance Assurance
Conducting regular audits is a critical strategy for ensuring compliance with healthcare vendor contracts. These audits serve as systematic evaluations of vendor performance, offering insights into their adherence to contractual obligations and regulatory requirements. For healthcare organisations, regular audits are not just best practices; they are necessities for maintaining care standards and safeguarding patient interests.
Audits should be structured to assess various aspects of vendor performance. This may include evaluating service delivery against agreed-upon metrics, reviewing compliance with data protection regulations, and examining vendor practices related to patient care. By conducting comprehensive audits, organisations can identify potential areas for improvement and proactively address compliance gaps.
In addition to enhancing compliance, regular audits foster transparency and accountability within vendor relationships. By cultivating a culture of openness and continuous improvement, organisations can encourage vendors to prioritise quality service delivery. This may involve providing feedback and support to vendors, enabling them to tackle challenges more effectively.
Moreover, the results of audits should be documented and communicated clearly to stakeholders within the organisation. This promotes a shared understanding of vendor performance and highlights any areas requiring corrective action. By integrating audit findings into strategic planning, healthcare organisations can make informed decisions about vendor relationships and ensure alignment with organisational goals.
Ultimately, regular audits are indispensable for monitoring compliance in healthcare vendor contracts. By prioritising these evaluations, organisations can safeguard patient care, strengthen vendor relationships, and enhance overall service delivery.
Establishing Performance Metrics for Accountability
Utilising performance metrics is a vital strategy for monitoring compliance with healthcare vendor contracts. These metrics provide quantifiable measures of vendor performance, allowing healthcare organisations to assess whether vendors meet the standards outlined in their contracts. By establishing clear metrics, organisations can ensure that vendors deliver quality services aligned with patient care objectives.
Performance metrics can encompass various aspects of vendor services, including response times, service quality, and patient satisfaction levels. For instance, a healthcare organisation may set targets for timely processing of patient referrals or maintaining certain standards in clinical outcomes. By measuring these metrics regularly, organisations can identify trends and areas for improvement, ensuring that vendors remain accountable for their performance.
In addition to enhancing compliance, performance metrics can facilitate constructive dialogue between healthcare organisations and vendors. Regular performance reviews provide opportunities for organisations to engage in discussions about vendor performance, addressing any challenges or concerns that may arise. This collaborative approach fosters a sense of partnership, encouraging vendors to prioritise quality service delivery.
Furthermore, organisations should consider integrating feedback mechanisms into performance metrics. Soliciting input from patients and staff can provide valuable insights into vendor performance, helping organisations refine their metrics and better align them with patient care objectives. By prioritising patient-centric metrics, organisations can enhance the overall quality of care delivered through vendor partnerships.
Ultimately, performance metrics are essential for monitoring compliance in healthcare vendor contracts. By utilising these measures effectively, organisations can ensure that vendors meet their expectations and contribute positively to patient outcomes.
Effective Reporting Mechanisms for Transparency
Establishing effective reporting mechanisms is essential for monitoring compliance with healthcare vendor contracts. These systems provide a structured framework for communicating performance data, regulatory compliance, and any issues that may arise during the vendor relationship. For healthcare organisations, robust reporting mechanisms enhance transparency and accountability, ensuring both parties remain informed and engaged.
Reporting mechanisms should be clearly defined within vendor contracts, outlining the frequency and format of performance reports. This may include regular updates on service delivery, compliance with regulatory standards, and any incidents or concerns that may impact patient care. By setting clear expectations for reporting, organisations can ensure that vendors provide timely and accurate information.
Moreover, organisations should encourage open communication channels that facilitate ongoing dialogue between healthcare providers and vendors. This may involve scheduled meetings or check-ins to discuss performance reports, address concerns, and collaboratively identify solutions to challenges that may arise. By fostering a culture of transparency, organisations can build trust and strengthen vendor relationships.
In addition to enhancing compliance, effective reporting mechanisms can support continuous improvement efforts. By analysing performance data and identifying trends over time, organisations can make informed decisions about vendor management, including adjustments to contracts or service delivery expectations. This proactive approach ensures that organisations remain agile in responding to changing healthcare needs.
Ultimately, establishing robust reporting mechanisms is vital for ensuring compliance in healthcare vendor contracts. By prioritising transparency and open communication, organisations can navigate the complexities of vendor relationships while safeguarding the quality of patient care.
Training and Education Initiatives for Staff
Implementing Contract Awareness Programs
Developing contract awareness programmes for healthcare staff is fundamental in ensuring compliance with vendor contracts. These programmes equip staff with the knowledge and understanding necessary to navigate the complexities of vendor relationships and uphold contractual obligations. For healthcare organisations, fostering awareness around vendor contracts is crucial for enhancing overall service delivery and patient care.
A well-structured contract awareness programme should address the essential components of vendor contracts, including performance expectations, compliance requirements, and the implications of non-compliance. By providing staff with a comprehensive understanding of these elements, organisations empower them to take an active role in monitoring vendor performance and ensuring adherence to contractual commitments.
Moreover, incorporating real-life scenarios and case studies into training sessions can enhance engagement and facilitate practical learning. Staff can explore challenges and successes experienced by other organisations in managing vendor relationships, gaining valuable insights that inform their practices. This experiential learning approach fosters a culture of continuous improvement and adaptability within the organisation.
Regular refreshers and updates on contract awareness are equally important. As regulations and organisational priorities evolve, staff must remain informed about any changes that may impact vendor relationships. By prioritising ongoing education, organisations can ensure that staff is equipped to navigate the dynamic landscape of healthcare vendor management effectively.
Ultimately, contract awareness programmes are a vital investment in ensuring compliance with vendor contracts. By equipping staff with the necessary knowledge and resources, organisations can foster a culture of accountability and excellence in service delivery.
Conducting Compliance Workshops for Knowledge Sharing
Organising compliance workshops represents an effective strategy to educate healthcare staff about vendor contracts and their associated compliance requirements. These workshops provide a forum for in-depth discussions, fostering a collaborative learning environment that encourages staff engagement and knowledge sharing. For healthcare organisations, investing in compliance workshops is essential for promoting a culture of accountability and regulatory adherence.
Workshops can cover a range of topics related to vendor contracts, including the key components of contracts, regulatory requirements, and best practices for monitoring compliance. By bringing together staff from various departments, organisations can foster cross-functional collaboration, enabling participants to share insights and experiences related to vendor management.
Incorporating interactive elements into workshops can enhance engagement and retention of information. Activities such as group discussions, case studies, and role-playing scenarios allow participants to apply their knowledge in practical settings. This experiential learning approach not only deepens understanding but also encourages participants to think critically about compliance challenges and solutions.
Moreover, inviting external experts or legal professionals to facilitate workshops can provide valuable insights into complex legal and regulatory topics. This expert guidance enhances the quality of the training and ensures that staff receives accurate and up-to-date information regarding compliance requirements.
Ultimately, compliance workshops are a vital tool for educating healthcare staff about vendor contracts and compliance obligations. By prioritising these workshops, organisations can cultivate a knowledgeable and engaged workforce committed to upholding regulatory standards.
Providing Ongoing Training for Continuous Improvement
Providing ongoing training for healthcare staff is crucial for ensuring continuous compliance with vendor contracts. The dynamic nature of the healthcare landscape necessitates that staff remain informed about changes in regulations, best practices, and contractual obligations. By prioritising ongoing training, healthcare organisations can foster a culture of excellence and adaptability in vendor management.
Training programmes should be regularly updated to reflect changes in legislation, industry standards, and organisational priorities. By incorporating these updates into training sessions, organisations can ensure that staff is equipped with the most current information regarding vendor compliance. This proactive approach helps to mitigate risks associated with non-compliance and enhances overall service delivery.
Moreover, ongoing training should encompass a variety of learning formats to cater to different learning styles. This may include online modules, in-person workshops, and interactive training sessions. By offering diverse training options, organisations can enhance engagement and ensure that staff remains motivated to participate in compliance training.
Additionally, creating opportunities for staff to share their experiences and insights can foster a culture of collaboration and continuous improvement. Establishing peer networks or discussion forums allows staff to engage in meaningful conversations about compliance challenges and share best practices for managing vendor relationships.
Ultimately, ongoing training is an essential investment in ensuring compliance with vendor contracts. By prioritising education and professional development, healthcare organisations can cultivate a knowledgeable and skilled workforce committed to delivering high-quality patient care.
Effective Risk Management in UK Healthcare Contracts
Identifying Potential Risks in Vendor Relationships
Identifying potential risks associated with healthcare vendor contracts is crucial for safeguarding patient care and ensuring compliance. Risks can emerge from various sources, including vendor performance issues, regulatory changes, and data protection challenges. For healthcare organisations, proactive risk identification is essential for mitigating challenges and securing positive outcomes in vendor relationships.
One effective strategy for identifying potential risks is conducting a comprehensive risk assessment at the outset of vendor engagement. This assessment should evaluate the specific risks linked to each vendor, considering factors such as their track record, compliance history, and the nature of the services provided. By understanding the unique risks posed by each vendor, organisations can tailor their management strategies accordingly.
Moreover, engaging staff in the risk identification process can provide valuable insights. Frontline staff often have direct interactions with vendors and can identify potential challenges that may arise in service delivery. Establishing open communication channels for staff to report concerns fosters a culture of vigilance and proactive risk management.
Regular reviews of existing vendor contracts can also help identify emerging risks. As regulations and market conditions evolve, organisations must ensure that their contracts remain relevant and robust. This may involve revisiting contractual terms related to performance expectations, compliance obligations, and termination clauses to address any potential vulnerabilities.
Ultimately, identifying potential risks in healthcare vendor contracts is a critical component of effective vendor management. By prioritising risk assessment and engaging staff in the process, organisations can enhance their ability to navigate challenges and secure positive outcomes for patient care.
Developing Robust Mitigation Strategies
Developing robust mitigation strategies is essential for addressing risks associated with healthcare vendor contracts. These strategies provide a proactive framework for managing potential challenges and ensuring compliance with contractual obligations. For healthcare organisations, effective risk mitigation is crucial for safeguarding patient care and maintaining the integrity of vendor relationships.
One key mitigation strategy involves establishing clear performance metrics within vendor contracts. By defining specific expectations and measurable outcomes, organisations can hold vendors accountable for their performance. This clarity not only enhances compliance but also provides a basis for evaluating vendor effectiveness over time.
Regular communication with vendors is another essential strategy for risk mitigation. Establishing open dialogue allows organisations to address concerns promptly and collaboratively identify solutions to challenges that may arise. By fostering a culture of transparency, organisations can build stronger partnerships with vendors and enhance overall service delivery.
In addition to communication, incorporating contingency planning into vendor management is vital. This may involve developing alternative plans for service delivery in the event of vendor performance issues or regulatory changes. By anticipating potential disruptions, organisations can ensure continuity of care and minimise the impact on patient services.
Furthermore, ongoing training and education for staff can enhance the effectiveness of mitigation strategies. Equipping staff with the knowledge and resources necessary to identify and address risks empowers them to take an active role in vendor management. This commitment to continuous improvement fosters a culture of accountability and supports optimal patient care.
Ultimately, developing robust mitigation strategies is essential for navigating the complexities of healthcare vendor contracts. By prioritising these strategies, organisations can proactively address risks, ensure compliance, and enhance overall service delivery.
Creating Contingency Plans for Unforeseen Circumstances
Establishing contingency plans is a critical aspect of risk management in healthcare vendor contracts. These plans outline the steps to be taken in the event of unforeseen circumstances, ensuring continuity of care and minimising disruptions to patient services. For healthcare organisations, effective contingency planning is essential for safeguarding patient welfare and maintaining the integrity of vendor relationships.
Contingency plans should be tailored to address specific risks associated with each vendor. This may involve developing protocols for service delivery in the event of vendor performance issues or regulatory changes. By anticipating potential challenges, organisations can ensure they are prepared to respond effectively, minimising the impact on patient care.
Moreover, involving key stakeholders in the contingency planning process enhances the robustness of these plans. Engaging staff from various departments, including clinical, operational, and administrative teams, ensures that the plans encompass all aspects of service delivery. This collaborative approach fosters a culture of preparedness and resilience within the organisation.
Regularly reviewing and updating contingency plans is equally important. As healthcare needs and regulatory requirements evolve, organisations must ensure that their plans remain relevant and effective. This might involve conducting simulations or tabletop exercises to test the effectiveness of contingency plans in real-world scenarios, allowing organisations to identify areas for improvement.
Ultimately, creating effective contingency plans is essential for managing risks associated with healthcare vendor contracts. By prioritising preparedness and fostering a culture of resilience, organisations can navigate challenges more effectively and ensure continuity of care for patients.
Legal Considerations for UK Vendor Contracts
Understanding Contract Law Basics
A solid understanding of the fundamentals of contract law is essential for healthcare organisations engaging with vendors. Contract law provides the legal framework governing the rights and obligations of parties involved in a contract, ensuring that agreements are enforceable and compliant with regulatory standards. For organisations navigating the complexities of vendor relationships, a firm grasp of contract law is vital for safeguarding their interests.
At its core, contract law encompasses the principles of offer, acceptance, consideration, and intention to create legal relations. Healthcare organisations must ensure that vendor contracts are structured to meet these legal requirements; failure to do so may result in unenforceable agreements. This includes ensuring that all parties clearly understand their roles and responsibilities within the contract.
Moreover, organisations should consider the implications of statutory regulations on contract law. Various laws govern healthcare contracts, including the Data Protection Act and the Health and Social Care Act, which impose specific obligations on parties involved in vendor relationships. By understanding these regulatory frameworks, organisations can ensure that their contracts align with legal requirements and protect patient interests.
Regularly reviewing and updating contracts is also crucial to reflect changes in legislation or organisational priorities. This proactive approach helps to maintain the relevance and enforceability of contracts, ensuring that healthcare organisations remain compliant in an evolving legal landscape.
Ultimately, a solid understanding of contract law basics is essential for healthcare organisations to navigate vendor relationships effectively. By prioritising legal compliance and ensuring that contracts are well-structured, organisations can safeguard their interests and enhance the quality of patient care.
Incorporating Dispute Resolution Mechanisms
Dispute resolution mechanisms are critical components of healthcare vendor contracts, providing a structured framework for addressing conflicts that may arise during the course of the relationship. These mechanisms ensure that disputes are resolved efficiently and fairly, minimising disruptions to patient care and maintaining the integrity of vendor relationships.
Incorporating clear dispute resolution processes into vendor contracts allows organisations to outline the steps to be taken in the event of a disagreement. This may involve specifying procedures for raising concerns, conducting investigations, and reaching resolutions. By establishing these processes upfront, organisations can mitigate the risk of prolonged conflicts and ensure timely resolution of issues.
Moreover, organisations should consider incorporating alternative dispute resolution (ADR) methods, such as mediation or arbitration, into vendor contracts. These methods offer a more flexible and collaborative approach to resolving disputes, often leading to quicker resolutions and reduced costs. By prioritising ADR, organisations can foster a more amicable environment for conflict resolution, preserving relationships with vendors.
Regular training and education for staff on dispute resolution processes can enhance the effectiveness of these mechanisms. Equipping staff with the knowledge and tools to manage disputes proactively empowers them to address conflicts at an early stage, minimising the potential for escalation.
Ultimately, incorporating effective dispute resolution mechanisms into healthcare vendor contracts is essential for safeguarding patient care and maintaining strong vendor relationships. By prioritising clear processes and promoting a culture of collaboration, organisations can navigate conflicts more effectively and enhance overall service delivery.
Ensuring Legal Compliance in Vendor Relationships
Ensuring legal compliance is a fundamental obligation for healthcare organisations engaging with vendors. Legal compliance encompasses adherence to various laws and regulations that govern vendor relationships, including contract law, data protection laws, and sector-specific regulations. For organisations, prioritising compliance is essential for safeguarding patient interests and maintaining the integrity of the healthcare system.
Organisations must conduct thorough due diligence before entering into vendor contracts, assessing the applicable legal and regulatory requirements. This includes reviewing the vendor’s compliance history and their ability to meet the specific obligations outlined in the contract. By understanding the legal landscape, organisations can make informed decisions about vendor partnerships and mitigate potential risks.
Moreover, integrating compliance monitoring into the vendor management process is crucial. Organisations should establish mechanisms for regularly assessing vendor compliance with legal obligations, including conducting audits and performance reviews. This proactive approach allows organisations to identify any areas of non-compliance and address them promptly, minimising the risk of legal repercussions.
Training and education for staff on legal compliance are also essential. Equipping employees with the knowledge and resources necessary to navigate legal complexities empowers them to take an active role in ensuring compliance. This commitment to ongoing education fosters a culture of accountability and supports optimal patient care.
Ultimately, ensuring legal compliance is a critical component of healthcare vendor contracts. By prioritising compliance and fostering a culture of accountability, organisations can navigate the complexities of vendor relationships while safeguarding patient interests and maintaining the integrity of the healthcare system.
Defining Clear Termination Clauses
The importance of termination clauses in healthcare vendor contracts cannot be overstated. These clauses provide a clear framework for ending the relationship between healthcare organisations and vendors, ensuring that the process is handled efficiently and transparently. For organisations, well-defined termination clauses are essential for protecting their interests and maintaining the quality of patient care.
Termination clauses should outline the specific grounds for termination, including performance failures, breaches of contract, or changes in regulatory compliance. By clearly articulating these conditions, organisations can take decisive action when vendor performance does not meet expectations. This not only safeguards the organisation’s interests but also ensures that patient care remains a priority.
Moreover, termination clauses should include provisions for notice periods and the obligations of both parties during the termination process. Clarity around these aspects minimises confusion and potential disputes, ensuring that all parties understand their rights and responsibilities. This transparency fosters a more amicable process, reducing the risk of conflicts during the termination phase.
Organisations should also consider the implications of termination on ongoing patient care. Contracts should stipulate protocols for ensuring continuity of care, minimising disruption to patients during vendor transitions. This may involve planning for handover procedures or identifying interim solutions to maintain service levels.
Ultimately, termination clauses are essential for safeguarding healthcare organisations and ensuring they have the flexibility to respond to challenges in vendor performance. By embedding these clauses in vendor contracts, organisations can proactively manage relationships and protect both their interests and the quality of patient care.
Understanding Data Protection Regulations
Understanding how data protection regulations, such as the General Data Protection Regulation (GDPR), impact healthcare vendor contracts is crucial for safeguarding patient information and ensuring compliance. These regulations impose specific obligations on organisations regarding the handling of personal data, making it essential for healthcare organisations to prioritise data protection in their vendor relationships.
Vendor contracts must explicitly require compliance with data protection laws, outlining the obligations vendors have regarding the collection, processing, and storage of personal data. This includes ensuring that vendors implement appropriate security measures to protect data from breaches or unauthorised access. Specific clauses may detail encryption standards, access controls, and incident response protocols to mitigate risks effectively.
Moreover, healthcare organisations should conduct thorough due diligence before engaging with vendors, assessing their data protection practices and history. This might involve reviewing compliance certifications or conducting audits to ensure they meet the necessary standards. Establishing a clear framework for monitoring vendor compliance throughout the contract’s duration is equally important, as it helps identify potential vulnerabilities and address them promptly.
Education and training around data protection compliance are essential for vendors. Healthcare organisations should provide resources and support to ensure that vendor staff understand their obligations under data protection laws. This commitment to ongoing education fosters a culture of compliance, enhancing the overall quality of service delivery.
By prioritising data protection compliance in vendor contracts, healthcare organisations can navigate the complexities of regulatory requirements while safeguarding patient information. This focus not only protects against potential legal repercussions but also reinforces the commitment to maintaining trust and integrity within the healthcare system.
Financial Considerations in UK Vendor Contracts
Budgeting Effectively for Compliance
Effective budgeting for compliance is a critical aspect of managing healthcare vendor contracts. Ensuring that vendors meet regulatory obligations and contractual commitments requires meticulous financial planning and resource allocation. For healthcare organisations, prioritising compliance-related budgeting is essential for safeguarding patient care and maintaining the integrity of vendor relationships.
Organisations should conduct a thorough assessment of the financial resources required to support compliance efforts. This includes accounting for expenses related to monitoring vendor performance, conducting regular audits, and investing in training and education for staff. By identifying these costs upfront, organisations can allocate sufficient resources to support ongoing compliance initiatives.
Moreover, organisations should consider the potential financial implications of non-compliance. Failure to meet regulatory obligations or contractual commitments can result in significant penalties, legal fees, and reputational damage. By proactively budgeting for compliance, organisations can mitigate these risks and protect their financial interests.
In addition to direct compliance costs, organisations should also consider the potential benefits of investing in compliance-related initiatives. Enhanced vendor performance and quality service delivery can lead to improved patient outcomes, ultimately resulting in cost savings and increased efficiency. By prioritising compliance in budgeting decisions, organisations can create a positive cycle that supports both financial sustainability and high-quality care.
Ultimately, effective budgeting for compliance is essential for navigating the complexities of healthcare vendor contracts. By prioritising financial planning and resource allocation, organisations can safeguard patient care and enhance the overall quality of service delivery.
Conducting a Cost-Benefit Analysis
Conducting a cost-benefit analysis for healthcare vendor contracts is a vital strategy for organisations seeking to optimise their vendor relationships and ensure compliance. This analysis allows organisations to evaluate the financial implications of engaging with a vendor against the expected benefits, promoting informed decision-making in vendor management.
To conduct a cost-benefit analysis, organisations should begin by identifying all costs associated with the vendor relationship. This includes direct costs, such as service fees and compliance-related expenses, as well as indirect costs, such as potential risks and the impact of vendor performance on patient care. By quantifying these costs, organisations can gain a clearer understanding of the financial implications of engaging with a particular vendor.
Next, organisations should assess the potential benefits of the vendor relationship. This may involve evaluating the expected improvements in service delivery, patient outcomes, and overall efficiency. By quantifying these benefits, organisations can determine whether the advantages of engaging with the vendor outweigh the associated costs.
Furthermore, organisations should consider the long-term implications of vendor relationships. This includes evaluating the potential for ongoing partnerships, the vendor’s reputation in the industry, and their ability to adapt to changing healthcare needs. By taking a holistic view of the vendor relationship, organisations can make informed decisions that support both compliance and organisational goals.
Ultimately, conducting a thorough cost-benefit analysis is essential for optimising healthcare vendor contracts. By prioritising financial evaluation and informed decision-making, organisations can enhance their vendor relationships and ensure compliance with regulatory obligations.
Implementing Robust Financial Reporting Mechanisms
Implementing robust financial reporting mechanisms is essential for monitoring compliance with healthcare vendor contracts. These systems provide a structured framework for tracking expenses, revenues, and financial performance related to vendor relationships. For healthcare organisations, effective financial reporting is crucial for ensuring transparency and accountability in vendor management.
Financial reporting should encompass all aspects of vendor relationships, including service fees, compliance-related costs, and any potential penalties associated with non-compliance. By maintaining comprehensive records, organisations can gain insights into the financial implications of vendor contracts and make informed decisions regarding resource allocation.
Moreover, regular financial reviews should be conducted to assess vendor performance in relation to financial metrics. This allows organisations to evaluate whether vendors are delivering the expected value for their services and identify any areas for improvement. By fostering a culture of accountability, organisations can encourage vendors to prioritise quality service delivery and compliance.
Incorporating financial reporting into the overall vendor management process also facilitates effective communication with stakeholders. By providing regular updates on financial performance and compliance status, organisations can ensure that key stakeholders remain informed and engaged in vendor management decisions.
Ultimately, implementing robust financial reporting mechanisms is essential for ensuring compliance in healthcare vendor contracts. By prioritising transparency and accountability, organisations can navigate the complexities of vendor relationships while safeguarding patient care and optimising financial outcomes.
Strategising for Effective Contract Negotiations
Developing effective contract negotiation strategies is crucial for securing favourable terms in healthcare vendor contracts. These strategies empower healthcare organisations to optimise their vendor relationships while ensuring compliance with regulatory obligations. By prioritising negotiation, organisations can protect their interests and enhance the overall quality of service delivery.
A key strategy for successful contract negotiations involves conducting thorough research on potential vendors. Understanding the vendor’s capabilities, reputation, and market position enables organisations to approach negotiations from a position of strength. By gathering relevant data, organisations can make informed decisions about the terms and conditions that best align with their goals.
Moreover, organisations should establish clear negotiation objectives, outlining the specific terms they wish to secure in the contract. This may include performance metrics, pricing structures, and compliance requirements. By articulating these objectives clearly, organisations can maintain focus during negotiations and advocate effectively for their interests.
Effective communication skills play a pivotal role in successful negotiations. Healthcare organisations should engage in active listening, seeking to understand the vendor’s perspective while articulating their own needs clearly. Building rapport and fostering a collaborative atmosphere can lead to more productive negotiations and mutually beneficial outcomes.
Additionally, organisations should consider leveraging competition among vendors to secure more favourable terms. By engaging multiple vendors and comparing their proposals, organisations can create a competitive environment that encourages vendors to offer better pricing, services, and compliance commitments.
Ultimately, developing effective contract negotiation strategies is essential for optimising healthcare vendor relationships. By prioritising research, clear objectives, effective communication, and competition, organisations can secure favourable terms that enhance compliance and support high-quality patient care.
Mitigating Financial Risks in Vendor Contracts
Identifying and mitigating financial risks associated with healthcare vendor contracts is critical for safeguarding organisational interests. Financial risks can arise from a variety of factors, including vendor performance issues, regulatory non-compliance, and unexpected costs. For healthcare organisations, proactive risk management is essential for ensuring compliance and maintaining the integrity of vendor relationships.
One effective strategy for mitigating financial risks is to establish clear performance metrics within vendor contracts. By defining specific expectations and measurable outcomes, organisations can hold vendors accountable for their financial performance. This clarity not only enhances compliance but also provides a basis for evaluating vendor effectiveness over time.
Regular communication with vendors is another essential strategy for financial risk mitigation. Establishing open dialogue allows organisations to address concerns promptly and collaboratively identify solutions to financial challenges that may arise. By fostering a culture of transparency, organisations can build stronger partnerships with vendors and enhance overall service delivery.
In addition to communication, incorporating contingency planning into vendor management is vital. This may involve developing alternative plans for service delivery in the event of vendor performance issues or regulatory changes. By anticipating potential financial disruptions, organisations can ensure continuity of care and minimise the impact on patient services.
Furthermore, ongoing training and education for staff can enhance the effectiveness of financial risk mitigation strategies. Equipping staff with the knowledge and resources necessary to identify and address financial risks empowers them to take an active role in vendor management. This commitment to continuous improvement fosters a culture of accountability and supports optimal patient care.
Ultimately, identifying and mitigating financial risks in healthcare vendor contracts is essential for navigating the complexities of vendor relationships. By prioritising proactive risk management, organisations can protect their financial interests and ensure compliance with regulatory obligations.
Technology Integration in UK Healthcare Vendor Contracts
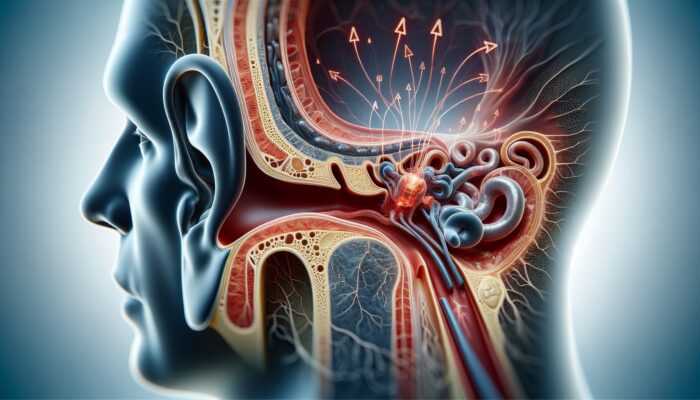
Impact of Electronic Health Records Systems
Understanding the impact of Electronic Health Records (EHR) systems on healthcare vendor contracts is vital in today’s digital landscape. EHR systems facilitate the efficient management of patient information and enhance service delivery but also introduce complexities related to data protection and compliance. For healthcare organisations, integrating EHR systems into vendor contracts requires careful consideration of regulatory obligations and best practices.
Vendor contracts must explicitly outline the responsibilities of vendors regarding EHR systems, including compliance with data protection laws and the secure handling of patient information. This includes stipulations around data encryption, access controls, and protocols for data sharing, ensuring that vendors implement robust security measures to protect against data breaches.
Moreover, organisations should establish clear expectations for the interoperability of EHR systems with other healthcare technologies. This involves defining how vendors will ensure that their systems integrate seamlessly with existing platforms, facilitating the smooth exchange of patient information across different care settings.
Regular assessments of EHR vendor performance are also essential for ensuring compliance and optimising service delivery. This may involve conducting audits of the vendor’s practices related to data handling, security measures, and system performance. By proactively monitoring vendor compliance, organisations can identify potential vulnerabilities and address them promptly.
Additionally, ongoing training and education for staff regarding EHR systems are crucial. Equipping staff with the knowledge and skills necessary to navigate EHR systems effectively empowers them to maximise the benefits of these technologies while ensuring compliance with regulatory obligations.
Ultimately, understanding the impact of EHR systems on healthcare vendor contracts is essential for safeguarding patient information and optimising service delivery. By prioritising compliance and integrating best practices, organisations can navigate the complexities of EHR vendor relationships while enhancing the quality of patient care.
Utilising Contract Management Software
Utilising contract management software is an effective strategy for improving the management of healthcare vendor contracts. These systems streamline the contract lifecycle, providing organisations with tools to create, monitor, and manage vendor agreements efficiently. For healthcare organisations, investing in contract management software is essential for ensuring compliance and optimising vendor relationships.
Contract management software offers a centralised platform for storing and organising vendor contracts, making it easier for organisations to access critical information and track compliance obligations. This centralisation enhances transparency and accountability, allowing organisations to monitor vendor performance and ensure adherence to regulatory requirements.
Moreover, contract management software often includes features for automating key processes, such as contract renewals and performance assessments. This automation reduces the administrative burden on staff, allowing them to focus on more strategic aspects of vendor management. By streamlining these processes, organisations can enhance overall efficiency and ensure that compliance obligations are met in a timely manner.
Regular training and education for staff on the effective use of contract management software are crucial. Equipping employees with the knowledge and skills necessary to navigate these systems empowers them to leverage technology effectively in managing vendor relationships. This commitment to ongoing education fosters a culture of accountability and supports optimal compliance outcomes.
Additionally, organisations should consider integrating contract management software with other healthcare technologies, such as EHR systems or financial reporting tools. This integration enhances data sharing and collaboration across departments, further improving the efficiency of vendor management processes.
Ultimately, utilising contract management software is essential for optimising the management of healthcare vendor contracts. By prioritising technology and investing in effective systems, organisations can enhance compliance and improve overall service delivery.
Implementing Data Security Measures
Implementing robust data security measures is a critical aspect of complying with healthcare vendor contracts. As healthcare organisations increasingly rely on technology for service delivery, the protection of sensitive patient information has become paramount. For organisations, prioritising data security is essential for safeguarding patient privacy and ensuring compliance with regulatory obligations.
Vendor contracts must explicitly outline the data security measures vendors must implement to protect patient information. This includes stipulations around encryption, access controls, and incident response protocols that vendors should have in place to mitigate the risk of data breaches. By establishing these requirements upfront, organisations can ensure that vendors are held accountable for safeguarding sensitive data.
Moreover, regular assessments of vendor data security practices are essential for ensuring compliance. Healthcare organisations should conduct audits and performance reviews to evaluate the effectiveness of vendors’ data security measures. This proactive monitoring allows organisations to identify potential vulnerabilities and address them promptly, minimising the risk of data breaches.
Additionally, ongoing training and education for staff regarding data security measures are crucial. Equipping employees with the knowledge and skills necessary to understand data protection obligations empowers them to take an active role in safeguarding patient information. This commitment to continuous education fosters a culture of accountability and enhances overall compliance outcomes.
Furthermore, organisations should consider integrating data security measures with broader risk management strategies. This may involve developing contingency plans for addressing potential data breaches or conducting simulations to test the effectiveness of security protocols. By prioritising data security within the context of overall risk management, organisations can ensure a comprehensive approach to compliance.
Ultimately, implementing robust data security measures is essential for complying with healthcare vendor contracts. By prioritising patient privacy and safeguarding sensitive information, organisations can navigate the complexities of vendor relationships while enhancing the quality of patient care.
Case Studies and Best Practices in UK Healthcare
Case Study 1: NHS Trust X’s Success in Vendor Management
In a recent case study involving NHS Trust X, the organisation successfully navigated the complexities of vendor relationships by implementing a robust vendor management framework. By prioritising compliance with regulatory standards and fostering strong partnerships with vendors, NHS Trust X enhanced the quality of care delivered to patients.
The organisation established clear performance metrics within vendor contracts, enabling them to monitor vendor performance effectively. Regular audits and performance reviews allowed NHS Trust X to identify areas for improvement and address any compliance gaps promptly. This proactive approach not only improved vendor accountability but also resulted in enhanced patient outcomes.
Moreover, NHS Trust X engaged staff in contract awareness programmes and compliance workshops, ensuring that employees were well-informed about vendor obligations. This commitment to education fostered a culture of accountability and compliance, empowering staff to take an active role in monitoring vendor performance.
Through these efforts, NHS Trust X achieved significant improvements in service delivery and patient satisfaction. The organisation’s focus on compliance and effective vendor management serves as a model for other healthcare organisations in the UK, highlighting the importance of prioritising regulatory adherence and collaboration in vendor relationships.
Case Study 2: Healthcare Group Y’s Risk Mitigation Strategy
A prominent private healthcare provider, Healthcare Group Y, faced significant challenges in managing vendor relationships due to compliance risks and performance issues. To mitigate these risks, the organisation implemented a comprehensive risk management strategy, resulting in improved vendor performance and enhanced patient care.
Healthcare Group Y began by conducting thorough risk assessments of their vendor partnerships, identifying potential vulnerabilities in service delivery and compliance. This proactive approach enabled the organisation to tailor their vendor management strategies to address specific risks effectively.
Additionally, Healthcare Group Y established clear communication channels with vendors, fostering open dialogue around performance expectations and compliance requirements. Regular meetings allowed both parties to address concerns promptly and collaboratively identify solutions to challenges.
Through ongoing training and education for staff, the organisation empowered employees to understand their roles in managing vendor relationships effectively. This commitment to education fostered a culture of accountability and vigilance, significantly reducing the risk of compliance issues arising from vendor partnerships.
As a result of these efforts, Healthcare Group Y achieved enhanced vendor performance, improved compliance outcomes, and ultimately, better patient care. This case study exemplifies the importance of proactive risk management and collaboration in navigating the complexities of healthcare vendor relationships.
Best Practice 1: Emphasising Continuous Improvement
One of the key best practices for managing healthcare vendor contracts is emphasising continuous improvement in vendor relationships. By fostering a culture of ongoing evaluation and enhancement, healthcare organisations can ensure that vendors consistently meet performance expectations and regulatory obligations.
To implement this practice, organisations should establish regular performance reviews that assess vendor effectiveness against agreed-upon metrics. This may involve soliciting feedback from staff and patients to identify areas for improvement and collaboratively developing action plans to address challenges.
Additionally, organisations should encourage vendors to participate in professional development opportunities, such as training programmes or industry conferences. By supporting vendors in enhancing their skills and knowledge, organisations can promote higher standards of service delivery and compliance.
Moreover, leveraging technology to monitor vendor performance can facilitate continuous improvement efforts. Implementing contract management software or performance tracking systems allows organisations to gather real-time data on vendor effectiveness, enabling proactive decision-making and swift identification of potential issues.
Ultimately, emphasising continuous improvement in vendor relationships is essential for optimising healthcare contracts and ensuring compliance. By prioritising this practice, organisations can enhance service delivery and achieve better patient outcomes.
Best Practice 2: Fostering Collaborative Partnerships
Fostering collaborative partnerships between healthcare organisations and vendors is another best practice for managing vendor contracts effectively. By creating a culture of collaboration and mutual support, organisations can enhance vendor performance and ensure compliance with regulatory obligations.
To promote collaborative partnerships, organisations should engage vendors in open communication regarding performance expectations and compliance requirements. Regular meetings and check-ins provide opportunities for both parties to address concerns and identify solutions collaboratively.
Moreover, organisations should encourage vendors to contribute to strategic planning efforts. By involving vendors in discussions around service delivery improvements or new initiatives, organisations can leverage their expertise and insights to enhance patient care.
Establishing joint goals and performance metrics can further strengthen collaborative partnerships. By aligning objectives, both parties can work together towards shared outcomes, fostering a sense of partnership and accountability.
Finally, recognising and celebrating vendor achievements can enhance collaboration and motivation. Acknowledging the contributions of vendors to patient care and organisational success fosters a positive working relationship and encourages ongoing commitment to service excellence.
Ultimately, fostering collaborative partnerships is essential for navigating the complexities of healthcare vendor contracts. By prioritising collaboration and mutual support, organisations can enhance vendor performance and ensure compliance, ultimately benefiting patient care.
Best Practice 3: Leveraging Technology for Compliance
Leveraging technology to enhance compliance in healthcare vendor contracts is a best practice that can significantly improve vendor management processes. By utilising digital tools and systems, organisations can streamline compliance monitoring, enhance data security, and optimise overall service delivery.
Implementing contract management software is a key strategy for improving compliance. These systems provide a centralised platform for managing vendor agreements, tracking performance metrics, and monitoring compliance obligations. By automating key processes, organisations can reduce administrative burdens and ensure timely adherence to regulatory requirements.
Moreover, utilising data analytics tools can enhance compliance monitoring by providing real-time insights into vendor performance and compliance status. Organisations can analyse performance data to identify trends and potential compliance gaps, enabling proactive decision-making and risk mitigation.
Additionally, organisations should consider investing in cybersecurity measures to protect sensitive patient information. Implementing robust data security protocols and conducting regular assessments can safeguard against data breaches and ensure compliance with data protection regulations.
Finally, ongoing training and education for staff on the effective use of technology is crucial for maximising compliance outcomes. Equipping employees with the knowledge and skills necessary to navigate digital tools empowers them to take an active role in ensuring compliance and optimising vendor management processes.
Ultimately, leveraging technology for compliance is an essential best practice in healthcare vendor management. By prioritising digital solutions and investing in effective systems, organisations can enhance compliance and improve overall service delivery.
Frequently Asked Questions (FAQs)
What are healthcare vendor contracts?
Healthcare vendor contracts are agreements between healthcare organisations and external suppliers that detail the services provided, compliance standards, and the obligations of both parties. These contracts are critical for ensuring quality service delivery and adherence to regulations.
Why is compliance important in healthcare vendor contracts?
Compliance is vital in healthcare vendor contracts to ensure that both parties meet legal, regulatory, and ethical standards. Non-compliance can result in penalties, legal issues, and compromised patient care.
What key components should be included in a healthcare vendor contract?
Key components of a healthcare vendor contract include service level agreements, termination clauses, confidentiality agreements, liability provisions, and data protection compliance measures.
How can healthcare organisations monitor vendor compliance?
Healthcare organisations can monitor vendor compliance through regular audits, performance metrics, and reporting mechanisms that track adherence to contractual obligations and regulatory requirements.
What role does staff training play in vendor compliance?
Staff training is crucial for ensuring that employees understand their roles in managing vendor relationships and compliance obligations. Ongoing education fosters a culture of accountability and supports optimal patient care.
How can healthcare organisations mitigate risks in vendor relationships?
Healthcare organisations can mitigate risks in vendor relationships by conducting thorough risk assessments, establishing clear performance metrics, and developing contingency plans to address potential challenges.
What technology can assist in managing healthcare vendor contracts?
Contract management software, data analytics tools, and EHR systems are essential technologies that can streamline vendor management processes, enhance compliance monitoring, and improve overall service delivery.
What should organisations do if a vendor fails to meet compliance standards?
If a vendor fails to meet compliance standards, organisations should initiate a review process, engage in open communication with the vendor, and implement corrective actions. If necessary, organisations may consider terminating the contract.
How can collaboration with vendors improve compliance?
Collaboration with vendors enhances compliance by fostering open communication, aligning objectives, and encouraging mutual accountability. This partnership approach promotes a shared commitment to quality service delivery.
What are the financial implications of vendor contracts?
Financial implications of vendor contracts include direct costs, such as service fees, as well as potential penalties for non-compliance. Effective budgeting and cost-benefit analyses are essential for managing these financial considerations.
The post Complying with Healthcare Vendor Contracts: Essential Guide appeared first on Healthcare Marketing Service.