Comprehensive Insights into the UK Healthcare System
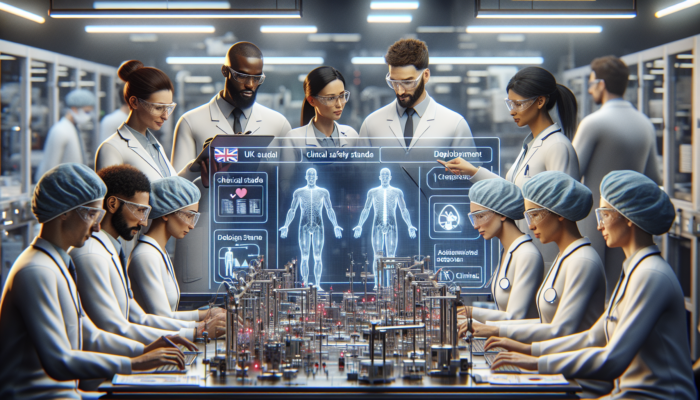
Exploring the Structure of the NHS
The National Health Service (NHS) in the United Kingdom is renowned as one of the most extensive and inclusive public healthcare systems globally. Established in 1948, the NHS is designed to provide healthcare services free at the point of delivery, primarily funded through taxation. The organisation is composed of several key entities, including NHS England, NHS Scotland, NHS Wales, and Health and Social Care in Northern Ireland. Each of these devolved administrations is responsible for managing its own healthcare services, ensuring that care is tailored to meet the specific needs and demands of local populations.
For example, NHS England oversees the commissioning and provision of healthcare services across England, focusing on primary care through General Practitioners (GPs) and hospitals. In contrast, NHS Scotland operates within a unique framework that prioritises primary care and community health services, reflecting the distinct healthcare challenges encountered in Scotland. The integration of health and social care services is particularly significant in Wales and Northern Ireland, where local governance plays an essential role in healthcare delivery, ensuring that services are responsive to community needs.
Grasping the intricate structure of the NHS is crucial for effectively implementing healthcare technology pilots. Stakeholders must adeptly navigate this complex landscape, aligning their technological solutions with the NHS’s overarching objectives while addressing the needs of both patients and healthcare professionals. The trajectory of healthcare technology in the UK will ultimately depend on how well these innovations can adapt to the established frameworks of the NHS.
Navigating the UK Healthcare Regulatory Framework
Successfully navigating the regulatory environment is essential for the effective implementation of healthcare technology pilots in the UK. The Care Quality Commission (CQC) and the Medicines and Healthcare products Regulatory Agency (MHRA) are two of the most significant regulatory bodies overseeing healthcare technology. The CQC ensures that healthcare providers maintain essential standards of quality and safety, fundamentally influencing any technology rollouts within the NHS.
The MHRA plays a vital role in regulating medical devices, ensuring their safety for use in patient care. Furthermore, adherence to the General Data Protection Regulation (GDPR) is crucial, especially concerning patient data. Any healthcare tech pilot must comply with these regulations to protect patient confidentiality and ensure ethical data usage, which is paramount in maintaining public trust.
Stakeholders should also be aware of the Digital Technology Assessment Criteria (DTAC), which provides a framework for assessing the effectiveness and safety of digital health technologies. This critical framework aids NHS organisations in making informed decisions regarding the adoption of new technologies, emphasising the need for robust evidence and patient outcome data to support these innovations.
Comprehending these regulatory aspects can significantly impact the success of healthcare technology pilots, as compliance with regulations not only builds trust with stakeholders but also safeguards patient welfare, making regulatory knowledge an essential prerequisite for any pilot initiative.
Engaging Stakeholders for Effective Technology Implementation
In the context of the UK healthcare system, engaging stakeholders is pivotal for the success of any tech pilot initiative. Key stakeholders include healthcare professionals, administrative staff, patients, and policymakers. Effective stakeholder engagement involves understanding the diverse perspectives and needs that each group brings to the table, which is essential for the pilot’s relevance.
Healthcare professionals can offer invaluable insights into the practical challenges encountered in daily operations within the NHS. Their involvement from the pilot’s inception ensures that the technology addresses real-world problems, contributing to higher acceptance rates among end-users. Engaging patients is equally important; their feedback helps guide the development of patient-centric solutions that enhance their care experience and ensure their needs are met.
Moreover, collaborating with regulatory bodies and local NHS organisations fosters a supportive environment for innovation. Stakeholder engagement strategies might include workshops, focus groups, and surveys to gather input and build consensus. By actively involving stakeholders throughout the pilot process, from planning to evaluation, organisations can align their tech solutions with the broader objectives of the NHS, ultimately facilitating smooth implementation and adoption of new technologies.
Identifying Opportunities for Healthcare Technology Pilots
Conducting a Comprehensive Needs Assessment
Identifying specific healthcare needs is foundational in determining how to implement healthcare tech pilots effectively. A comprehensive needs assessment is essential for pinpointing gaps within the current healthcare delivery system, enabling organisations to target their tech solutions effectively. This process often involves analysing existing patient pathways, reviewing clinical outcomes, and consulting healthcare professionals across various specialities to ensure all needs are considered.
Engaging with data sources such as Public Health England and local Clinical Commissioning Groups (CCGs) can yield insights into prevalent health issues within a given population. Techniques such as stakeholder interviews and surveys can further identify the day-to-day challenges faced by healthcare providers and patients alike. For instance, if a hospital identifies a significant backlog in appointment scheduling, a tech solution that streamlines booking processes could be developed and piloted to alleviate this issue.
Additionally, examining national health priorities, such as the NHS Long Term Plan, can help align tech pilots with broader health initiatives. Understanding local health inequalities is also vital; technology can be tailored to address specific demographic challenges, ensuring that interventions are both relevant and necessary for the communities served.
By conducting a thorough needs assessment, stakeholders not only justify their tech pilot’s existence but also enhance the chances of successful implementation and positive patient outcomes, ultimately driving improvements in healthcare delivery.
Strategically Selecting Appropriate Technology
Choosing the appropriate technology for healthcare pilots requires a strategic approach that aligns with the identified needs of the NHS. Factors influencing technology selection include the scalability of the solution, interoperability with existing systems, and the potential to improve patient outcomes and operational efficiencies.
Innovative solutions such as telehealth platforms, electronic health records (EHRs), and patient management systems have shown great promise in enhancing healthcare delivery. However, the technology must also align with the digital maturity of the healthcare providers involved. For instance, a solution may be highly effective in a technologically advanced trust but may struggle in an environment that still relies heavily on paper-based records.
Collaboration with technology vendors is critical in this phase. Engaging with suppliers who understand the unique challenges of the NHS can lead to tailored solutions that fit seamlessly into existing workflows and enhance operational efficiencies. Furthermore, pilot technologies must undergo rigorous testing to ensure they meet regulatory standards before implementation, safeguarding patient safety and compliance.
Ultimately, the objective is to select technology that not only meets immediate needs but also has the potential for long-term integration into broader healthcare practices, ensuring that innovations can continue to evolve alongside the healthcare landscape, driving continual improvements in patient care.
Conducting Thorough Feasibility Studies
Conducting feasibility studies is an indispensable step in the process of how to implement healthcare tech pilots effectively. These studies help assess the practicality of the proposed technology, informing stakeholders about potential challenges and resource requirements that may arise during implementation.
A well-structured feasibility study typically includes an evaluation of technical, economic, legal, operational, and scheduling factors. Technical feasibility looks at whether the technology can be integrated into existing systems and whether the necessary infrastructure is in place to support its use. Economic feasibility analyses cost implications, considering both short-term investment and long-term savings associated with the technology.
Legal feasibility is crucial, particularly in the UK, where compliance with data protection laws like GDPR is non-negotiable. Operational feasibility assesses whether the pilot aligns with current clinical workflows and whether staff possess the necessary skills to implement and utilise the technology effectively. This ensures that the pilot can be executed smoothly and with minimal disruption to existing services.
Moreover, conducting pilot simulations can provide insights into potential operational challenges. Engaging with frontline staff during this phase enables organisations to anticipate hurdles and develop tailored training and support mechanisms, ensuring a smoother transition upon actual implementation. The insights gained from these simulations can be invaluable in fine-tuning the pilot’s approach.
Feasibility studies culminate in a comprehensive report that helps stakeholders make informed decisions, highlighting the likelihood of success and areas that may require additional consideration before launching the pilot. This thorough analysis is essential for minimising risks and enhancing the chances of successful implementation.
Engaging Stakeholders in the Pilot Development Process
As with the earlier phase, stakeholder engagement remains a central theme when identifying opportunities for healthcare tech pilots. Engaging stakeholders not only generates buy-in but also fosters collaboration that enhances the pilot’s relevance and effectiveness in addressing specific healthcare challenges.
Different engagement strategies can be employed, including community consultations, online platforms for feedback, and collaborative workshops. Engaging patients, healthcare professionals, and administrative staff ensures that diverse perspectives are considered, ultimately leading to a more comprehensive understanding of the needs that the technology must address.
Building a coalition of supportive stakeholders can also facilitate access to resources, funding, and expertise necessary for the pilot’s success. It is essential to create a transparent communication strategy to keep stakeholders informed of developments and gather ongoing feedback during the pilot’s lifecycle. This transparency fosters trust and encourages active participation.
Moreover, leveraging existing networks, such as NHS Innovation Hubs, can enhance stakeholder engagement efforts. These hubs can provide invaluable resources and connections to other healthcare entities facing similar challenges. By fostering an inclusive environment, organisations can ensure that the technology developed meets the nuanced needs of the UK healthcare landscape, ultimately improving patient outcomes.
Securing Financial Support and Resources
Exploring Diverse Funding Sources for Healthcare Tech Pilots
Securing funding for healthcare tech pilots in the UK can be a complex but manageable task if approached strategically. Various funding sources are available, ranging from government grants to private investment and philanthropic contributions. The NHS Innovation and Technology Payment (ITP) programme, for instance, is designed to support the adoption of innovative technologies within the NHS, providing a valuable resource for pilot funding.
Local Clinical Commissioning Groups (CCGs) may also have specific funds allocated for innovation within their geographical areas. Engaging with these bodies early in the process can yield insights into available funding streams that align with the proposed pilot’s objectives. Additionally, partnerships with academic institutions can open doors to research grants and collaborative funding opportunities that can bolster financial support.
Crowdfunding has also emerged as a viable funding option for healthcare innovations, allowing organisations to tap into community support for novel technologies. However, it is essential to maintain transparency and demonstrate the potential value of the technology to attract financial backing from supporters and stakeholders alike.
Ultimately, leveraging a combination of these funding sources can provide the financial stability needed to launch and sustain tech pilots, facilitating the effective implementation of innovative solutions that improve care delivery and patient outcomes across the NHS.
Strategic Resource Allocation for Successful Pilot Implementation
Resource allocation is a critical aspect of ensuring the success of healthcare tech pilots in the UK. It involves determining the necessary human, technological, and financial resources required to implement and sustain the pilot effectively. A thorough assessment of project requirements is essential for understanding the scope and scale of the pilot.
This includes not only financial resources for the technology itself but also the personnel required for training, support, and ongoing evaluation of the pilot’s effectiveness. Engaging with stakeholders to identify existing resource gaps will aid in the efficient distribution of responsibilities and tasks among team members, ensuring that all aspects are covered.
Consideration must also be given to the technological infrastructure needed to support the pilot. This may require investment in additional hardware, software, or network capabilities. Ensuring that the selected technology is compatible with existing systems is crucial for a seamless integration process that minimises disruptions.
Moreover, creating a clear project timeline that outlines key milestones can help guide resource allocation effectively. Regular reviews of resource use can identify areas of overspend or underutilisation, enabling adjustments that ensure the pilot remains on track and within budget. This strategic approach to resource management is vital for the pilot’s success.
A well-planned approach to resource allocation not only enhances pilot implementation but also increases the likelihood of achieving desired outcomes, ultimately contributing to the successful adoption of healthcare tech pilots that enhance patient care.
Effective Budget Management for Healthcare Technology Initiatives
Effective budget management is integral to the successful implementation of healthcare tech pilots in the UK. A detailed budget should encompass all projected costs associated with the pilot, including technology acquisition, personnel training, marketing, and ongoing maintenance. This comprehensive financial planning is crucial for ensuring that all aspects of the pilot are adequately funded.
Establishing a clear financial plan at the outset will provide a roadmap for managing resources throughout the pilot. Regular monitoring of spending against the budget helps identify potential overruns early, allowing for timely adjustments and reallocations where necessary. This proactive approach to budget management helps mitigate the risk of financial shortfalls that could jeopardise the pilot’s success.
In addition, reporting mechanisms should be established to provide stakeholders with regular updates on financial progress. Transparent communication regarding budget management fosters trust and encourages continued stakeholder engagement and support throughout the pilot’s lifecycle.
Implementing cost-saving measures, such as in-kind contributions from partners or shared services, can also enhance budget management. By being strategic and resourceful, organisations can maximise their funding and achieve significant impact with their technology pilots, ultimately benefiting patient care and healthcare delivery.
Crafting Comprehensive Pilot Proposals
Structuring a Compelling Pilot Proposal
Crafting a compelling pilot proposal is essential for gaining support and funding for healthcare tech initiatives. A well-structured proposal should begin with an executive summary that succinctly outlines the pilot’s objectives, the technology involved, and the anticipated outcomes, capturing the attention of stakeholders from the outset.
Following the summary, a detailed description of the identified healthcare needs should be presented, accompanied by data and evidence supporting the necessity of the proposed solution. This section is crucial in convincing stakeholders of the pilot’s relevance and potential impact on patient care, ensuring that their concerns are addressed.
The proposal should also include a comprehensive project plan that outlines timelines, milestones, and resource requirements. Additionally, a clearly defined budget is essential, detailing the financial aspects and highlighting potential funding sources that can be tapped into.
Incorporating an evaluation plan within the proposal is also vital. This plan should specify how success will be measured, including key performance indicators (KPIs) and data collection methods. Lastly, a transparent communication strategy outlining how stakeholders will be engaged throughout the pilot will enhance the proposal’s credibility and foster collaborative efforts, ensuring that everyone is on board with the initiative.
A well-structured proposal not only serves as a roadmap for the pilot but also acts as a persuasive tool for securing stakeholder buy-in and funding, ultimately increasing the likelihood of successful implementation.
Leveraging Data and Evidence to Strengthen Proposals
Incorporating relevant data and evidence into pilot proposals significantly strengthens their credibility and impact. Stakeholders are more likely to support initiatives that are backed by robust data illustrating the need for change and the effectiveness of the proposed technology in addressing specific healthcare challenges.
Utilising existing research, case studies, and statistical analyses can provide a solid foundation for the proposal. For instance, demonstrating how similar technologies improved patient outcomes in other NHS trusts can lend weight to the proposed pilot, making it more compelling to decision-makers. Additionally, presenting data on current challenges faced by healthcare providers in the specific context of the proposed pilot can help clarify the necessity of the intervention and its potential benefits.
Engaging in partnerships with academic institutions can enhance the proposal by integrating empirical research and evaluation methods. These collaborations can provide access to additional data sources and expertise in rigorous evaluation techniques, further bolstering the proposal’s credibility.
Ultimately, the inclusion of data and evidence not only bolsters the rationale for the pilot but also provides a framework for measuring success, ensuring that the initiative remains aligned with the overarching goals of the NHS and contributes positively to patient care.
Understanding Approval Processes for Pilot Projects
Navigating the approval processes for healthcare tech pilots in the UK can be a complex endeavour. Each NHS organisation may have its own protocols, necessitating a thorough understanding of local processes and requirements to ensure a smooth approval journey.
Typically, proposals must undergo a formal review process involving clinical governance committees, finance departments, and potentially external stakeholders. Engaging with these bodies early in the proposal development phase can streamline the approval process, as their feedback can inform the proposal’s content and structure, making it more robust and aligned with organisational goals.
It is essential to prepare for possible challenges during the approval process. This may involve addressing concerns around data privacy, technology integration, and resource allocation. Being proactive and providing comprehensive evidence to support the pilot’s safety, effectiveness, and compliance with regulations can facilitate smoother approvals and build trust with decision-makers.
Moreover, maintaining clear communication with stakeholders throughout the approval process is vital. Regular updates and opportunities for feedback can foster a sense of ownership and collaboration, ultimately accelerating the journey from proposal to pilot launch and enhancing stakeholder engagement.
Fostering Stakeholder Engagement in Proposal Development
As with previous sections, effective stakeholder engagement remains a cornerstone of developing pilot proposals. Engaging stakeholders in the proposal process not only builds support but also enriches the proposal with diverse perspectives and insights, which is critical for addressing the multifaceted challenges within the healthcare system.
Collaborating with healthcare professionals, patients, and administrative staff to gather input on the proposal’s content can enhance its relevance and applicability. This collaborative approach fosters trust and demonstrates a commitment to addressing the needs of all parties involved, which is essential for gaining support.
Creating a stakeholder engagement plan that outlines how and when stakeholders will be involved can also streamline this process. This plan should include regular meetings, opportunities for feedback, and mechanisms for ongoing communication throughout the pilot’s lifecycle, ensuring stakeholders remain informed and engaged.
Additionally, leveraging existing networks, such as NHS Innovation Hubs, can enhance outreach efforts, connecting with a broader audience and fostering collaborative possibilities that benefit the proposal’s success. By prioritising stakeholder engagement, organisations can create pilot proposals that resonate with the needs of the healthcare community, increasing the likelihood of securing approval and funding for their initiatives.
Strategic Budget Planning for Pilot Initiatives
Developing a comprehensive budget plan for healthcare tech pilots is a critical component of ensuring their success. A well-structured budget should encompass all costs associated with the pilot, including technology acquisition, training, staffing, and ongoing operational expenses. This thorough financial planning is essential for ensuring that all aspects of the pilot are adequately funded.
Involving financial experts in the budgeting process can provide a clearer understanding of potential costs and help identify areas where savings can be made. Additionally, presenting a detailed budget breakdown to stakeholders enhances transparency and demonstrates responsible financial planning, fostering trust and confidence in the pilot.
Creating a contingency plan within the budget is also essential. This plan should outline how unforeseen costs will be managed, ensuring that the pilot remains financially viable even in the face of unexpected challenges. A proactive approach to financial management is crucial for minimising risks.
Moreover, establishing a clear timeline for expenditures can help manage cash flow effectively. Regular financial reviews and updates can identify any potential budgetary issues early, allowing for timely interventions and adjustments to keep the pilot on track.
A meticulous approach to budget planning not only helps ensure that pilots are financially sustainable but also builds trust with stakeholders, reinforcing the commitment to responsible resource management and the successful implementation of healthcare tech pilots.
Executing Healthcare Pilot Projects Effectively
Essential Project Planning for Successful Implementation
Effective project planning is the backbone of successful healthcare tech pilot implementation. A well-thought-out project plan serves as a roadmap, detailing timelines, milestones, and responsibilities that ensure all team members are aligned toward common goals and objectives.
Kick-off meetings involving all stakeholders set the tone for the project and clarify expectations. These meetings create an opportunity to discuss roles and responsibilities while establishing a collaborative atmosphere that encourages open communication and teamwork throughout the pilot’s lifecycle.
The project plan must also outline strategies for risk management. Identifying potential risks and devising mitigation strategies early in the process can significantly reduce the impact of unforeseen challenges, ensuring that the project remains on track.
Utilising project management tools can enhance planning efforts, enabling teams to track progress, manage timelines, and allocate resources efficiently. Regular status updates and review meetings can keep the project on track, ensuring that any deviations from the plan are addressed promptly and effectively.
Ultimately, a robust project plan lays the groundwork for successful implementation, enhancing the likelihood of achieving desired outcomes in the pilot and contributing positively to patient care.
Seamless Technology Integration in Healthcare Settings
Integrating technology into UK healthcare settings poses unique challenges that must be addressed to ensure successful implementation. Achieving seamless integration requires careful consideration of existing workflows, systems, and personnel capabilities, ensuring that the technology complements rather than disrupts current practices.
Collaboration with IT departments is critical during this phase. Engaging technical experts can provide insights into system compatibility, data migration processes, and security considerations, ensuring that the new technology aligns with existing infrastructure and supports operational efficiencies.
Training staff on the new technology is essential for successful integration. Creating tailored training programmes that account for the varying levels of digital literacy among staff will enhance user adoption and confidence in utilising the new systems effectively. Ongoing support mechanisms, such as helplines and user guides, can further bolster this process, ensuring that staff feel adequately supported.
Pilot testing the technology before full-scale implementation can identify potential issues and facilitate troubleshooting, ensuring that the technology operates as intended. Gathering feedback during this phase allows for immediate adjustments, paving the way for a smoother transition when the pilot officially launches.
Overall, successful technology integration hinges on thorough planning, collaboration, and support, ultimately maximising the potential benefits of the pilot and enhancing patient care across the NHS.
Providing Comprehensive Training and Support
Ensuring adequate training and support for pilot project teams is vital to the success of healthcare technology initiatives. A well-structured training programme tailored to the specific needs of users significantly enhances technology adoption rates and overall project success, empowering staff to utilise the new systems effectively.
Training initiatives should begin well before the pilot’s launch. Providing comprehensive onboarding sessions that cover both the technical aspects of the technology and its practical application in real-world scenarios will empower staff to utilise the new system effectively and with confidence.
Utilising a train-the-trainer model can also be beneficial. By equipping a select group of staff members with in-depth knowledge of the technology, they can serve as resources for their colleagues during the pilot, fostering a culture of knowledge sharing and support that enhances the overall implementation process.
Continuous support mechanisms must be established to assist staff throughout the pilot. This might include dedicated helpdesks, online resources, and regular check-ins to address questions or concerns that arise during implementation. Ensuring that staff feel supported will enhance their confidence and encourage successful technology adoption.
By prioritising training and support, organisations can create a positive environment that encourages technology adoption, ultimately leading to improved patient care and pilot success across the healthcare system.
Monitoring and Evaluating Pilot Effectiveness
Monitoring and evaluating pilot projects is essential for assessing their impact and effectiveness in the UK healthcare landscape. Establishing clear metrics for success allows organisations to track progress and identify areas for improvement, ensuring that the pilot aligns with its intended goals and objectives.
Key performance indicators (KPIs) should be defined at the outset of the pilot, aligning with the overall goals of the project. These could encompass patient outcomes, operational efficiencies, and user satisfaction, providing a comprehensive view of the pilot’s success and areas for enhancement.
Data collection methods must be robust and systematic. Employing both qualitative and quantitative approaches can provide a comprehensive view of the pilot’s performance. Surveys, interviews, and focus groups can yield valuable insights from users, while data analytics tools can track quantitative metrics, offering a well-rounded understanding of the pilot’s impact.
Regular evaluation meetings should be scheduled to review findings and discuss progress. These collaborative sessions provide an opportunity to celebrate successes and address challenges proactively, enabling timely interventions as needed to keep the project on track and aligned with its objectives.
Ultimately, a commitment to thorough monitoring and evaluation not only demonstrates accountability but also informs future scaling efforts, ensuring that successful pilots can be replicated across the NHS and contribute positively to patient care.
Engaging Stakeholders Throughout Implementation
Continuous stakeholder engagement during the implementation phase is crucial to the success of healthcare tech pilots. Keeping stakeholders informed and involved fosters a sense of ownership and commitment to the project, ultimately enhancing the likelihood of successful adoption and integration of the technology.
Regular communication updates, such as newsletters and progress reports, can keep stakeholders engaged and informed about key developments. These updates should highlight both achievements and challenges, providing a transparent view of the pilot’s progress and fostering trust among all parties involved.
Encouraging feedback from stakeholders throughout the implementation process not only builds trust but also enables organisations to make real-time adjustments based on user experiences. This iterative approach allows for fine-tuning the technology and its deployment, maximising its effectiveness and ensuring it meets the needs of users and patients.
Organising workshops and focus groups can also facilitate deeper engagement and collaboration. These forums provide opportunities for stakeholders to share their insights and experiences, contributing to a more comprehensive understanding of the pilot’s impact and identifying potential areas for improvement.
By prioritising stakeholder engagement during implementation, organisations can cultivate a supportive environment that enhances the chances of pilot success and paves the way for future innovations in healthcare technology.
Evaluating and Monitoring Pilot Outcomes
Defining Key Performance Metrics for Evaluation
Defining key performance indicators (KPIs) is a critical step in monitoring and evaluating healthcare tech pilots. These metrics provide a quantitative framework for assessing the pilot’s effectiveness and measuring the impact of the technology on patient care and operational efficiencies.
When establishing KPIs, it is essential to align them with the overall objectives of the pilot. For example, if the pilot aims to reduce patient wait times, metrics could include average wait time before consultation, patient throughput rates, and patient satisfaction scores, all of which provide valuable insights into the pilot’s success.
Incorporating both short-term and long-term metrics ensures a comprehensive evaluation. Short-term metrics can indicate immediate effects, while long-term metrics assess sustained impacts on patient care and system efficiencies, providing a complete picture of the pilot’s effectiveness.
Engaging stakeholders in the discussion of performance metrics can foster a shared understanding of success and facilitate buy-in across the organisation. Regularly reviewing these metrics allows for iterative improvements throughout the pilot, ensuring that goals remain aligned with real-world outcomes and organisational priorities.
Ultimately, a well-defined set of performance metrics not only guides the evaluation process but also provides a basis for decision-making regarding the future of the pilot and its potential for scaling across the NHS.
Implementing Effective Data Collection Strategies
Effective data collection methods are vital for successfully evaluating healthcare tech pilots. Employing a combination of qualitative and quantitative approaches provides a comprehensive view of the pilot’s impact and effectiveness, ensuring that all relevant aspects are captured.
Quantitative data can be gathered through various means, such as electronic health records (EHRs), patient surveys, and operational reports. This data helps to identify trends and measure performance against the established KPIs, offering valuable insights into the pilot’s outcomes and overall effectiveness.
Qualitative data, on the other hand, can be sourced through interviews, focus groups, and open-ended survey questions. This type of data captures the experiences and opinions of users, providing context and depth to the quantitative findings, which enhances the overall evaluation process.
Implementing a systematic approach to data collection is essential for ensuring that data is reliable, valid, and ethically gathered. Engaging stakeholders in the data collection process can also enhance participation and trust, encouraging honest feedback and active involvement in the evaluation.
Regularly analysing and synthesising collected data allows organisations to assess the pilot’s performance and identify areas for improvement. This ongoing evaluation fosters a culture of learning and adaptability, ultimately contributing to the pilot’s success and scalability across the healthcare sector.
Effectively Reporting Pilot Results to Stakeholders
Effectively reporting pilot results is critical for communicating the outcomes of healthcare tech initiatives to stakeholders. A well-structured report should include a detailed analysis of the data collected, highlighting key findings and insights gained throughout the pilot’s lifecycle, providing a comprehensive overview for decision-makers.
Clear and concise visualisations, such as charts and graphs, can enhance the presentation of data, making it more accessible and engaging for diverse audiences. Accompanying these visuals with narrative explanations provides context for the findings, aiding in comprehension and interpretation of the results.
In addition to presenting quantitative results, it is vital to include qualitative insights from stakeholders and users. Highlighting personal stories and testimonials can humanise the data and illustrate the real-world impact of the technology on patient care, making the report more relatable and persuasive.
Recommendations for future action should also be included in the report, based on the findings and insights gained from the evaluation process. This forward-looking approach demonstrates a commitment to learning and improvement, fostering continued stakeholder support for future initiatives and enhancing the potential for scaling successful pilot projects.
Ultimately, a comprehensive and well-crafted report not only serves as a valuable resource for stakeholders but also lays the groundwork for successful scaling and replication of effective healthcare tech pilots across the NHS.
Strategies for Scaling Successful Pilot Projects
Extracting Key Lessons from Pilot Experiences
Identifying key lessons from successful healthcare tech pilots is crucial for informing future scaling efforts. Reflecting on both successes and challenges encountered during the pilot can provide valuable insights into what works and what doesn’t in the context of the NHS, shaping future initiatives.
Conducting post-pilot evaluations that involve all stakeholders allows for a comprehensive analysis of the pilot’s outcomes. This collaborative approach encourages open dialogue, ensuring that diverse perspectives are considered when identifying lessons learned, leading to more informed decision-making in the future.
Key areas of focus during this reflective process include technology usability, training effectiveness, stakeholder engagement, and overall project management. Understanding which factors contributed to success can help organisations replicate these elements in future pilots, while identifying challenges allows for proactive mitigation strategies in subsequent initiatives.
Additionally, documenting case studies of successful pilots can serve as powerful tools for sharing lessons learned with other organisations. These case studies can highlight best practices, effective strategies, and potential pitfalls to avoid, contributing to a culture of learning and innovation across the NHS and improving the overall quality of patient care.
By embracing lessons learned from pilot projects, organisations can enhance their capacity for scaling successful initiatives and driving meaningful improvements in patient care across the healthcare system.
Developing Effective Expansion Strategies
Developing effective expansion strategies for scaling successful healthcare tech pilots requires a thorough understanding of the pilot’s outcomes and the broader healthcare landscape. A strategic approach considers various factors, including local needs, resource availability, and stakeholder support, which are vital for successful implementation in new settings.
Engaging with stakeholders during the expansion planning phase is essential, ensuring that their insights and concerns inform the scaling strategy. This collaborative approach fosters buy-in and support, which is crucial for successful implementation in new settings and facilitates smoother transitions.
Identifying potential partners, such as other NHS trusts or community health organisations, can facilitate expansion efforts. Collaborating with these entities allows for resource sharing, knowledge exchange, and enhanced reach, ultimately increasing the impact of the technology and improving patient outcomes.
Moreover, developing a phased approach to scaling can mitigate risks associated with larger rollouts. This might involve piloting the technology in smaller settings before expanding to broader populations, allowing organisations to refine their approach based on real-world feedback and ensuring that the technology is ready for wider application.
Ultimately, a well-considered expansion strategy enhances the likelihood of successfully scaling successful healthcare tech pilots, contributing to improved patient outcomes and operational efficiencies across the NHS, and supporting the overall goals of the healthcare system.
Communicating Success and Future Plans to Stakeholders
Communicating pilot success and scaling plans to stakeholders is vital for maintaining support and fostering collaboration. A clear communication strategy that outlines key achievements, lessons learned, and future goals ensures stakeholders remain informed and engaged in the ongoing initiatives.
Utilising various communication channels, such as newsletters, presentations, and community meetings, allows for reaching diverse audiences. Tailoring messages to specific stakeholder groups is essential, ensuring that the information resonates with their unique interests and concerns, which can enhance receptivity to future initiatives.
Highlighting patient stories and quantitative outcomes can effectively demonstrate the pilot’s impact, reinforcing the value of continued investment in healthcare technology. These success stories serve as powerful testimonials to the effectiveness of the technology, helping to cultivate ongoing support from both internal and external stakeholders and fostering a culture of innovation.
Regular updates on the scaling process keep stakeholders informed and engaged, fostering a sense of ownership and collaboration. Encouraging feedback and input during this phase demonstrates a commitment to inclusivity and transparency, ultimately enhancing the chances of successfully scaling the pilot and driving improvements in patient care within the NHS.
By prioritising stakeholder communication, organisations can build strong relationships that support the expansion of successful healthcare tech pilots, ultimately driving improvements in patient care within the UK healthcare system.
Addressing Challenges in Healthcare Technology Pilots
Navigating Regulatory Hurdles in Implementation
Addressing regulatory challenges is an essential part of navigating the implementation of healthcare tech pilots in the UK. The regulatory landscape can be complex, with multiple agencies involved in overseeing various aspects of healthcare technology and ensuring patient safety and compliance.
Understanding the specific regulations that apply to the pilot is crucial. Compliance with the Care Quality Commission (CQC) standards, data protection regulations like GDPR, and the requirements set forth by the Medicines and Healthcare products Regulatory Agency (MHRA) is non-negotiable. Failing to adhere to these regulations can lead to significant delays or even the abandonment of the pilot, jeopardising the potential benefits of the technology.
Engaging with regulatory bodies early in the planning process and throughout implementation can help clarify requirements and expectations. Establishing open communication channels allows for ongoing dialogue, enabling organisations to navigate any regulatory hurdles that may arise and ensuring compliance is maintained.
Additionally, collaborating with legal experts can provide valuable insights into compliance issues and risk management strategies. By proactively addressing regulatory challenges, organisations can ensure a smoother implementation process, ultimately enhancing the likelihood of pilot success and the effective deployment of technology within the healthcare system.
Overcoming Technical Issues During Implementation
Overcoming technical issues is a common challenge faced during healthcare tech pilot implementations. Ensuring that the chosen technology integrates seamlessly with existing systems is critical for facilitating smooth operations and minimising disruptions to patient care.
Conducting thorough testing before the pilot launch can help identify potential technical issues that may arise during implementation. This could involve simulation testing or trial runs that allow stakeholders to experience the technology in action and provide feedback, ensuring that any issues are addressed prior to full rollout.
Engaging IT support from the outset is vital for addressing any technical glitches quickly. Having dedicated technical resources available during implementation can minimise disruptions and enhance user confidence in the new technology, contributing to a successful adoption process.
Additionally, creating a troubleshooting guide and providing ongoing support for end-users can help mitigate challenges associated with technology adoption. By being proactive and responsive to technical issues, organisations can foster a positive experience that encourages successful implementation and enhances the overall effectiveness of the pilot.
Ultimately, a commitment to addressing technical challenges enhances the likelihood of pilot success and contributes to the long-term sustainability of the technology within the healthcare system, ensuring that innovations can be effectively utilised to improve patient care.
Implementing Effective Change Management Strategies
Managing change effectively is crucial for ensuring successful outcomes in healthcare tech pilots. The introduction of new technologies can create resistance among staff, making it essential for organisations to implement effective change management strategies that facilitate smooth transitions.
Communicating the rationale behind the pilot and its potential benefits to all stakeholders is vital for fostering buy-in. Highlighting how the technology aligns with the overall goals of the NHS and improves patient care can motivate staff to embrace the changes and actively participate in the pilot.
Involving stakeholders in the planning and implementation phases can also mitigate resistance. By soliciting feedback and encouraging collaboration, organisations can create a sense of ownership among staff, making them more likely to support the pilot and contribute to its success.
Training and support initiatives are critical components of effective change management. Providing comprehensive training ensures staff feel confident using the new technology, while ongoing support mechanisms, such as help desks or peer assistance, can help address concerns as they arise, fostering a supportive environment for technology adoption.
By prioritising change management, organisations can navigate the complexities of implementing new technologies, ultimately enhancing the likelihood of pilot success and achieving meaningful improvements in patient care across the healthcare landscape.
Enhancing Stakeholder Engagement During Implementation
Effective stakeholder engagement remains a key challenge when implementing healthcare tech pilots. Engaging stakeholders throughout the process not only builds trust but also fosters collaboration that enhances the pilot’s relevance and effectiveness in meeting healthcare needs.
Creating a stakeholder engagement plan that outlines how and when stakeholders will be involved can streamline this process. This plan should include regular meetings, opportunities for feedback, and mechanisms for ongoing communication throughout the pilot’s lifecycle, ensuring that stakeholders remain informed and engaged.
Understanding the diverse needs and perspectives of stakeholders allows organisations to tailor their engagement strategies effectively. Engaging patients, healthcare professionals, and administrative staff ensures that diverse perspectives are considered, ultimately leading to a more comprehensive understanding of the needs that the technology must address.
Utilising platforms for transparent communication, such as newsletters or digital forums, keeps stakeholders informed and involved, reinforcing a sense of collaboration. Additionally, recognising and celebrating stakeholder contributions can foster a supportive environment that enhances the chances of pilot success and encourages ongoing engagement in future initiatives.
Ultimately, prioritising stakeholder engagement throughout the pilot process allows organisations to cultivate strong partnerships that support and enhance healthcare tech initiatives, ultimately benefiting patient care across the NHS.
Addressing Funding Constraints for Innovation
Securing adequate funding for healthcare tech pilots is a challenge that many organisations face. Financial constraints can limit the scope and effectiveness of technology initiatives, making it essential to explore diverse funding options that can support innovation in patient care.
Engaging with local Clinical Commissioning Groups (CCGs), NHS Innovation and Technology Payment (ITP) programmes, and philanthropic contributions can create a multifaceted approach to funding. Understanding the specific interests and priorities of potential funders can help tailor proposals that resonate with their objectives and increase the likelihood of securing necessary financial support.
Additionally, leveraging existing resources and partnerships can enhance funding capacity. Collaborating with academic institutions and industry partners can provide access to grants, shared resources, and other financial support that can alleviate funding constraints and support the pilot’s success.
Implementing a phased approach to funding can also mitigate risks. By piloting technology in smaller, manageable phases, organisations can demonstrate effectiveness and build a case for additional funding as they progress through the implementation process, ensuring that financial challenges do not hinder innovation.
Ultimately, a proactive and strategic approach to securing funding can enhance the feasibility and success of healthcare tech pilots, ensuring that financial challenges do not impede the pursuit of innovation in patient care.
Frequently Asked Questions
What constitutes a healthcare tech pilot?
A healthcare tech pilot is a trial project designed to test new technologies in real-world healthcare settings, assessing their effectiveness, feasibility, and impact on patient care and operational efficiency.
Why is stakeholder engagement crucial in tech pilots?
Stakeholder engagement is critical as it fosters collaboration, builds trust, and ensures that the technology meets the needs of healthcare professionals and patients, enhancing the likelihood of successful implementation and adoption.
What types of funding are available for healthcare tech pilots in the UK?
Funding sources include government grants, NHS Innovation and Technology Payments, private investments, philanthropic contributions, and potential crowdfunding opportunities, offering diverse financial support for innovative initiatives.
What key performance indicators should be measured in a pilot?
KPIs may include patient outcomes, operational efficiencies, user satisfaction, and adoption rates, all of which provide insights into the pilot’s effectiveness and impact on healthcare delivery.
How can organisations ensure compliance with regulations during tech pilots?
Organisations can ensure compliance by engaging with regulatory bodies, understanding relevant regulations, and conducting thorough assessments of how the technology aligns with legal requirements, ensuring that patient safety is prioritised.
What is the role of feasibility studies in pilot projects?
Feasibility studies assess the practicality of proposed technology, examining technical, economic, legal, and operational factors to determine whether the pilot is viable in its intended context, ultimately guiding decision-making.
How can organisations manage change during tech implementation?
Effective change management involves clear communication, stakeholder involvement, comprehensive training, and ongoing support, fostering a positive environment for technology adoption and ensuring smooth transitions.
What is the importance of monitoring and evaluation in tech pilots?
Monitoring and evaluation provide a framework for assessing outcomes, informing necessary adjustments, and identifying lessons learned, ensuring that the technology meets its intended goals and continuously improves patient care.
How can successful pilots be scaled effectively?
Scaling successful pilots involves developing strategic expansion plans, engaging stakeholders, identifying potential partners, and conducting phased rollouts to mitigate risks associated with larger implementations.
What challenges do healthcare tech pilots typically encounter?
Common challenges include regulatory hurdles, technical issues, funding constraints, and resistance to change, all of which can impact the pilot’s success if not addressed proactively and strategically.